A Walkthrough Of The LifeDNA Vitamins & Supplements Report
Aira
on
August 16, 2024
Overview
What Is A Dietary/Food Supplement?
A food supplement, or a dietary supplement, is designed to provide nutrients or compounds that a person might not be sufficiently consuming. These supplements can include vitamins, minerals, amino acids, antioxidants, enzymes, and herbs. They are available as tablets, capsules, powders, and liquids. While they can support a balanced diet, they are not intended to replace whole foods or be a sole source of nutrition. Instead, they ensure that an individual’s nutrient intake meets their body’s demands for proper functioning, especially when their diet lacks specific nutrients.

Are Food Supplements Healthy?
Food supplements can be healthy when used appropriately and with a clear understanding of their purpose. They are beneficial in filling nutritional gaps and supporting specific health needs when dietary intake is insufficient. However, they are not a cure-all and should not be a substitute for a balanced and varied diet. Excessive or inappropriate use of supplements can lead to health issues, including nutrient imbalances and unwanted interactions with medications. Therefore, it is vital to use supplements judiciously, under the guidance of a healthcare professional, and as part of an overall healthy lifestyle.
Why We Need Food Supplements?
We may need food supplements to address specific nutritional deficiencies or to meet increased nutrient demands that isn’t fulfilled just through diet. Factors such as aging, health conditions, dietary restrictions, or special life stages (like pregnancy or intense physical training) can increase the need for certain nutrients. In such cases, supplements are the practical means to ensure adequate nutrient intake. However, it is essential to acknowledge that supplements are an adjunct to, not a substitute for, a well-rounded diet, and their use should be based on individual nutritional requirements and under professional guidance.
What Food Supplements Should You Take?
The need for food supplements varies largely among individuals, depending on diet, lifestyle, age, health status, and specific nutritional needs. It is best to consult with a healthcare professional or a registered dietitian to assess your dietary intake and determine if you have any nutritional gaps that require supplementation. Generally, they may recommend appropriate supplements if your diet lacks certain nutrients, such as Vitamin D during the winter months, or calcium for bone health. However, indiscriminate use of supplements can lead to unnecessary intake and potential nutrient imbalances, so personalized advice is crucial.
Are Fortified Foods Better Than Supplements?
Fortified foods can offer a more food-based approach to increasing the intake of specific nutrients and are beneficial in improving the overall nutrient profile of the diet without the need to take pills or capsules. They can be helpful in reaching populations with specific nutrient deficiencies and are often part of public health strategies to address those deficiencies. However, the advantage of fortified foods over supplements depends on individual dietary patterns, nutritional needs, and preferences. While fortified foods can seamlessly integrate nutrients into the diet, supplements can provide higher, more targeted doses of specific nutrients when needed. Both approaches have their place in a comprehensive strategy to meet nutritional needs.
Why Can't Supplements Replace Food?
Supplements cannot replace food because whole foods provide a complex nutritional matrix that supplements cannot replicate. Along with vitamins and minerals, food also contains fiber, antioxidants, and numerous other bioactive compounds that work together to promote health. The interaction of these compounds within the body’s biological systems contributes to proper digestion, absorption, and the holistic functioning of the human body. Moreover, the experience of eating—tasting, digesting, and metabolizing whole foods—plays a crucial role in satiety, appetite regulation, and the enjoyment of meals, aspects that supplements alone cannot fulfill.
Impact Of Dietary/Food Supplements
Proper use, tailored to individual health needs and based on scientific evidence, can support disease prevention, immune function, and overall physical and mental performance. However, the balance is key, as indiscriminate use without professional guidance might lead to unintended consequences. As such, dietary supplements represent a valuable tool in the modern health landscape, promising benefits when integrated thoughtfully into a holistic approach to health and wellness.
What Foods And Supplements Lower Cholesterol?
Foods rich in soluble fiber, such as oats, barley, beans, lentils, fruits, and vegetables, can help lower cholesterol levels. Omega-3 fatty acids, found in fish like salmon and mackerel, flaxseeds and walnuts, have been shown to lower triglycerides and improve heart health. Supplements such as red yeast rice, psyllium husk, and plant sterols can also help reduce cholesterol levels. However, it’s crucial to use these supplements under medical supervision, as they can interact with medications and might not be suitable for everyone.
Which Food Supplement Is Best For Bodybuilding?
Protein supplements are popular for bodybuilding as they support muscle repair and growth. Whey protein is a favorite due to its high biological value and fast absorption. Creatine is another widely used supplement known for improving strength, increasing lean muscle mass, and helping muscles recover quickly during exercise. Other supplements like branched-chain amino acids (BCAAs), beta-alanine, and L-glutamine can also support muscle recovery and growth. However, it’s essential to approach supplementation with a strategy that complements a well-planned diet and workout routine, and ideally, under the guidance of a fitness or health professional.
The LifeDNA Vitamins & Supplements Report
The LifeDNA Vitamins & Supplements Report offers a comprehensive and personalized analysis designed to unlock the secrets of your genetic makeup about nutrition and supplement needs.
This cutting-edge report delves into how your unique DNA influences your body’s requirement for various vitamins, minerals, and other essential nutrients, ensuring you can make informed decisions about your diet and supplement intake.
By understanding your genetic predispositions, the report empowers you to optimize your health and well-being, guiding you towards a more tailored and fruitful approach to nutrition and overall lifestyle choices.
Whether you seek to enhance your fitness routine, boost your mental clarity, or maintain a balanced and healthy life, the LifeDNA Vitamins & Supplements Report is your gateway to a more personalized health journey.
Learn more here.
Vitamin C Levels refer to the concentration of vitamin C, or ascorbic acid, in the body. This essential nutrient is vital for growth, development, and repair of body tissues. It is involved in many body functions, including collagen formation, iron absorption, proper functioning of the immune system, wound healing, and maintenance of cartilage, bones, and teeth. Low levels can lead to conditions like scurvy, while adequate levels are paramount for overall health. Vitamin C levels are significantly influenced by genetics.
A 2010 study found that a specific genetic variant, rs33972313 (C/T), located in the SLC23A1 gene (which encodes a vitamin C transporter), is significantly associated with lower levels of l-ascorbic acid in the blood.
Read more: The Genetics of Vitamin C Levels
Vitamin E Levels indicate the amount of vitamin E, a group of fat-soluble compounds with antioxidant properties, in the body. It is crucial for maintaining healthy skin and eyes and strengthening the body’s natural defense against illness and infection (the immune system). Vitamin E also plays a role in cellular communication and the formation of red blood cells.
In-Depth: The Genetics of Vitamin E Needs
Vitamin A Levels refer to the concentration of vitamin A in the body, a fat-soluble vitamin essential for vision, the immune system, and reproduction. Vitamin A also helps the heart, lungs, kidneys, and other organs work properly.
Vitamin A levels have significant genetic roots. For example, genetic variations in the TRR gene have been linked to vitamin A levels in the body. The TTR gene is responsible for coding the transthyretin protein. Transthyretin plays a crucial role in distributing vitamin A and the hormone thyroxine across the body.
Read about this and other interesting genetic markers here.
Vitamin B5 Levels, also known as pantothenic acid levels, refer to the concentration of this vitamin in the body. Vitamin B5 is essential for energy production, the synthesis of fatty acids, and the metabolism of fats, proteins, and coenzyme A. Read in detail about the genetics of vitamin B5 levels here.
Vitamin B6 Levels indicate the concentration of vitamin B6, or pyridoxine, in the body. It is involved in the metabolization processes of protein, fats, and carbohydrates. It further aids in new red blood cells formation and supports the function of the nervous and immune systems.
Vitamin B6 levels have been shown to vary based on variations in genes like ALPL and NBPF3.
Vitamin B12 Levels measure the amount of vitamin B12, a crucial nutrient for nerve tissue health, brain function, and the production of red blood cells. Deficiency can lead to anemia and neurological issues.
Vitamin B9 (Folate) Levels indicate the concentration of folate or folic acid, a B vitamin necessary for proper brain function, plays a crucial role in mental and emotional health. It is also essential for producing DNA and RNA and particularly important in aiding rapid cell division and growth, such as during infancy and pregnancy.
Vitamin B9 levels in the body are strongly associated with genetic variations in the MTHFR gene. The MTHFR gene is a prominent gene that influences several critical functions related to growth and development. We will discuss the functions of this gene in more detail in a future article, stay tuned!
Vitamin D Levels refer to the concentration of vitamin D, a fat-soluble vitamin essential for strong bones because it helps the body use calcium from the diet. Traditionally, vitamin D deficiency has been linked to rickets, a disease in which the bone tissue does not properly mineralize, leading to soft bones and skeletal deformities.
The GC gene, which codes for the vitamin D Binding Protein, a pivotal player in vitamin D level regulation, is closely tied to how vitamin D influences our wellness.
Read in more detail: The Genetics of Vitamin D Levels
Vitamin K Levels indicate the concentration of vitamin K in the body. It is crucial for blood clotting and bone health. It plays a key role in helping the blood clot, and preventing excessive bleeding. It is also needed for bone proteins.
Studies on the genetics of vitamin K levels are still ongoing. Two genes are of special interest, the gene coding for VKORC1, which has a role in vitamin K processing and the gene for GGCX, which encodes an enzyme that activates vitamin K-dependent protein.
Read in more detail: How Your Genes Affect Vitamin K Levels
Zinc Levels refer to the bodily concentration of zinc, a critical mineral for a healthy immune system, wound healing, DNA synthesis, and cell division. Zinc also supports regular growth and development during pregnancy, childhood, and adolescence. We require zinc also for proper sense of taste and smell.
Zinc levels have a genetic component. Studies have found variations in genes like PPCDC and CA1 to influence blood zinc levels.
Iron Levels denote the amount of iron in the body, an essential mineral critical for the production of hemoglobin, a protein in red blood cells that carries oxygen from the lungs to the rest of the body. Iron is also necessary for growth, development, normal cellular functioning, and for synthesizing some hormones and connective tissue.
Genetic variations in genes like HFE and TMPRSS6 influence iron levels.
Cholesterol Levels traits (two of them) refer to the amount of cholesterol in the blood, either the low-density lipoprotein (LDL, or “bad” cholesterol) or the high-density lipoprotein (HDL, or “good” cholesterol). While cholesterol is essential for forming cell membranes, certain hormones, and vitamin D, high LDL cholesterol levels increase the risk of heart disease and stroke.
Genetic factors play a significant role in determining an individual’s HDL cholesterol levels. Read about it here.
Copper Levels indicate the concentration of copper in the body, a trace mineral vital for making red blood cells and maintaining nerve cells and the immune system. It also helps the body form collagen, absorb iron, and play a role in energy production.
The SNP rs1175550, located in the SMIM1 gene, is linked to serum copper concentrations. Individuals carrying the A allele of this SNP are more susceptible to lower levels of copper.
DHA Levels refer to the amount of docosahexaenoic acid, a type of omega-3 fatty acid that is a major structural component of the human brain, cerebral cortex, skin, and retina. Adequate DHA levels are crucial for brain health, visual development, and reducing inflammation.
From the genetic perspective, variations in the ELOVL2 gene, responsible for producing proteins that extend the chain length of omega-3 and omega-6 fatty acids, have been linked to reduced levels of DHA. This connection is significant, considering the crucial part DHA plays in maintaining brain health and supporting cognitive functions.
Liver Enzyme Levels refer to the concentrations of the liver enzymes, including alanine-aminotransferase (ALT), aspartate transaminase (AST), alkaline phosphatase (ALP), and gamma-glutamyl transferase (GGT). These enzymes are released into the bloodstream when the liver is damaged. Monitoring these levels helps diagnose and monitor liver damage or diseases.
A 2008 GWAS across three populations (7,715 individuals) and validated in three additional cohorts (4,704 individuals) identified specific genetic loci associated with levels of liver enzymes, including ALT, GGT, and ALP. Significant loci were discovered for ALT (on chromosomes 10 and 22), one for GGT (on chromosome 12), and three for ALP (on chromosomes 1, 6, and 10). The study also confirmed known associations with GGT and ALP levels.
CoQ10 Levels refer to the amount of Coenzyme Q10 in the body, a substance that helps convert food into energy and acts as a powerful antioxidant, protecting cells from damage and playing a part in the metabolism.
Genetics significantly influences CoQ10 levels. A 2016 study investigated the genetic factors influencing serum CoQ10 levels. A meta-analysis of two Northern German cohorts identified two significant genetic loci linked to CoQ10 levels. The COLEC12 gene on chromosome 18 and the NRXN-1 gene on chromosome 2, previously associated with neuronal diseases, showed the strongest associations.
Probiotic Need reflects the necessity for probiotics, live beneficial bacteria and yeasts that are good for the digestive system. They help keep the gut healthy and are often referred to as “good” or “friendly” bacteria because they help keep the gut environment healthy.
A 2016 study examined how genetics influences the gut microbiome by analyzing metagenomic sequencing data from 1,514 individuals. Researchers identified significant genetic associations with microbial species, pathways, and gene ontology categories, pinpointing nine loci linked to microbial taxonomies and 33 loci associated with microbial pathways and gene ontology terms. The study also highlighted 32 loci, related to complex diseases, immunity, and food preferences, with a suggestive association level. Notably, the findings include new associations, like those at the genome-wide significance for CLEC4F–CD207 and CLEC4A–FAM90A1.
Magnesium Levels indicate the amount of magnesium in the body, an essential mineral for bone health and proper function of nerves, muscles, etc. Magnesium is also involved in over 300 biochemical reactions in the body.
Variations in the TRPM6 and ATP2B1 genes are commonly associated with changes in magnesium levels and an increased likelihood of developing hypomagnesemia.
Thyroid Function refers to how well the thyroid gland works, producing hormones that regulate metabolism, heart rate, body temperature, and more. Tests often measure levels of Thyroid Stimulating Hormone (TSH), T3, and T4 to assess thyroid function.
Genetics significantly influence thyroid hormone levels, TSH concentrations, and the likelihood of developing autoimmune thyroid diseases. Studies indicate that genetic factors account for nearly 67% of the variation in thyroid hormone and TSH levels. While research has identified specific genes, like those for phosphodiesterase 8B (PDE8B), iodothyronine deiodinase 1 (DIO1), F-actin-capping protein subunit beta (CAPZB), and the TSH receptor, as contributors to these variations, they explain only a little portion of the hormone level differences. More genes and genetic mechanisms affecting thyroid hormone levels remain undiscovered.
Melatonin Levels measure the concentration of melatonin, a hormone the pineal gland produces to regulate the sleep-wake cycle. It is often called the “sleep hormone” as high levels can help you fall asleep.
Genetics significantly influences melatonin levels. For example, the MTNR1B gene variant is linked to endogenous melatonin signaling, sleep status, and circadian rhythm.
Calcium Levels indicate the amount of calcium in the body, essential for maintaining strong bones and carrying out many vital functions such as muscle contraction, blood clotting, and nerve transmission.
Phosphorus Levels measure the amount of phosphorus, or phosphate, in the body, an essential mineral involved in hundreds of cellular activities everyday. The body uses phosphorus to repair cells and tissues, to make the energy needed for daily activities, and to filter waste out of the kidneys.
Glomerular Filtration Rate (GFR) is a test to check how well the kidneys work. It estimates how much blood passes through the glomeruli, tiny filters in the kidneys, each minute. Several genetic factors contribute to GFR regulation, influencing the efficiency of the glomerular filtration process.
For example, genetic variants in SHROOM3, such as the SNP rs17319721, have been linked to an increased risk of Chronic Kidney Disease (CKD) and reduced GFR.
Read in more detail: Understanding the Genetics of Glomerular Filtration Rate
Proteinuria refers to the presence of abnormal amounts of protein in the urine, often a sign of kidney damage. It is not normal to have protein in the urine, and its presence can be an early sign that the kidneys are not working correctly.
Genetic studies have unraveled several genetic markers related to proteinuria. Read about it in more detail here: Proteinuria- Unravelling The Clues in Your Urine
Visual Acuity measures the clarity or sharpness of vision. It is a quantitative measure of the ability to identify black symbols on a white background at a standardized distance as being separate entities.
Genome-wide association studies on visual acuity have revealed several candidate genetic markers linked to visual acuity. We go into more details of these studies in this article.
To unlock the full list of traits, get started with the LifeDNA Vitamins & Supplements report. Learn more here.
Why LifeDNA?
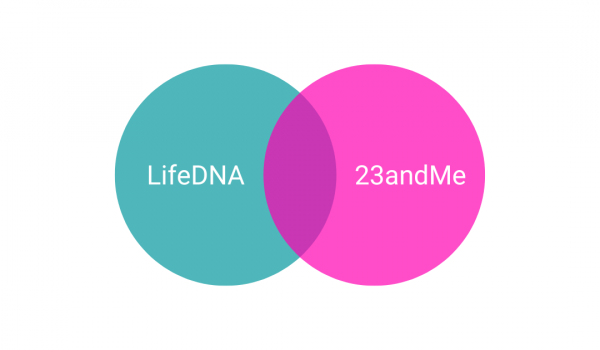
LifeDNA has emerged as a prominent option for analyzing 23andMe and many other raw DNA data, owing to a combination of unique offerings and a commitment to personalized wellness.
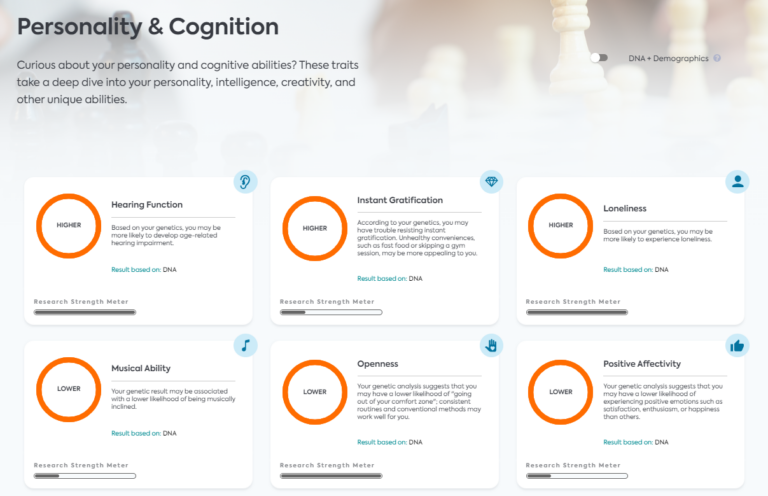
We offer a basic DNA raw data analysis package to kickstart your journey. Users with raw data from 23andMe, AncestryDNA, etc., can access 194+ traits across interests such as Nutrition, Wellness, Vitamins and Supplements, Personality, Fitness, Sleep, Methylation, and Skincare.
Further, if you do not have raw DNA data, such as from 23andMe, LifeDNA provides that too. Start your personalized wellness journey with LifeDNA’s state-of-the-art DNA kits here.
Here is why many regard LifeDNA as the best option for making the most of your 23andMe, AncestryDNA, and other raw data:
- Holistic Approach to Wellness: Unlike many other platforms that focus strictly on health-related risks or ancestry, LifeDNA adopts a holistic approach. We analyze genetic data to offer personalized optimizations for nutrition (including a customized grocery list!), skin care, vitamins & supplements, wellness, personality & cognition, and fitness. This range lets users get a complete picture of their wellness needs based on their DNA.
- Product Recommendations: We go beyond just providing insights. We offer specific product recommendations, skincare ingredients, or supplements tailored to an individual’s genetic profile. It makes our service actionable, allowing users to make immediate changes based on their results.
- Data Security: At LifeDNA, we emphasize on protecting user data. Our commitment to privacy ensures that users can trust the platform with their sensitive genetic information.
- User-Friendly Reports: LifeDNA reports are easy to interpret. We have designed our reports to be accessible to the layperson without compromising on the depth and accuracy of the information.
- Continual Updates: As genetic research evolves, so does LifeDNA’s platform. Users can expect their reports and insights to be up-to-date with the latest scientific findings.
- Dedicated Research and Development: At LifeDNA, we invest in research to continually refine our algorithms, ensuring that we base the insights on cutting-edge science.
- Educational Resources: LifeDNA also provides ample resources for users to understand their genetic makeup better. This education-first approach demystifies the complex world of genetics, making it approachable and actionable for everyone.
- Scientific rigor: To create an unmatched commitment to scientific rigor, LifeDNA partners with CLIA-certified, CAP-accredited, and HIPAA-compliant laboratories.
References
- https://www.sciencedirect.com/science/article/pii/S0002916523019160
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4317173/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10054309/
- https://pubmed.ncbi.nlm.nih.gov/22147956/
- https://www.gbhealthwatch.com/Nutrient-Magnesium-Genes.php
- https://www.nature.com/articles/ng.3663
- https://dx.doi.org/10.1093/hmg/ddw134
- https://www.cell.com/ajhg/fulltext/S0002-9297(08)00502-8
- https://journals.plos.org/plosgenetics/article?id=10.1371/journal.pgen.1002193
- https://doi.org/10.1093/hmg/ddt239
- http://dx.doi.org/10.1007/s12263-015-0474-2
- https://pubmed.ncbi.nlm.nih.gov/20621035/
- https://www.nature.com/articles/s41467-017-02662-2
- https://doi.org/10.1016/j.ajhg.2009.02.011
- https://doi.org/10.1093/hmg/ddp428
- https://www.sciencedirect.com/science/article/pii/S0002916523019160
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6520936/
- https://ods.od.nih.gov/factsheets/ExerciseAndAthleticPerformance-HealthProfessional/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8949037/
- https://www.mayoclinic.org/diseases-conditions/heart-disease/in-depth/omega-3/
*Understanding your genetics can offer valuable insights into your well-being, but it is not deterministic. Your traits can be influenced by the complex interplay involving nature, lifestyle, family history, and others.
Our reports have not been evaluated by the Food and Drug Administration. The contents on our website and our reports are for informational purposes only, and are not intended to diagnose any medical condition, replace the advice of a healthcare professional, or provide any medical advice, diagnosis, or treatment. Consult with a healthcare professional before making any major lifestyle changes or if you have any other concerns about your results. The testimonials featured may have used more than one LifeDNA or LifeDNA vendors’ product or reports.