Mitochondrial DNA Levels and Genetics
Aira
on
August 12, 2024
Mitochondria, the tiny powerhouses inside our cells, hold unique instructions for making them – the mitochondrial DNA (mtDNA). Unlike the DNA in our nucleus, which comes from both parents, mtDNA is inherited solely from your mother. But how much mtDNA do our cells have, and why does it matter?
What is Mitochondrial DNA?
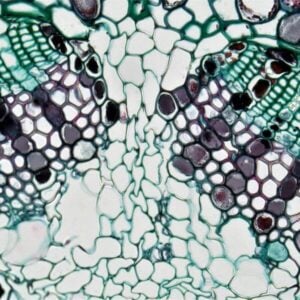
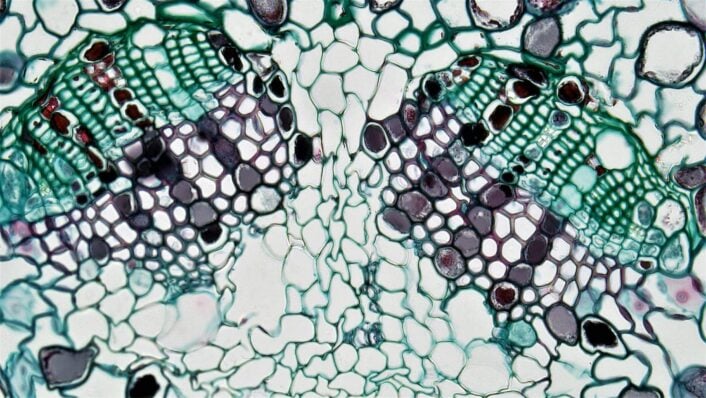
Mitochondrial DNA or mtDNA is a small circular chromosome tucked away within mitochondria. These organelles are essential for cellular function, acting like tiny factories that convert the energy from food into a usable form for our cells: the adenosine triphosphate (ATP).
Compared to the massive encyclopedia of our nuclear DNA, mtDNA is a tiny pamphlet. It contains a mere 16,569 base pairs, encoding just 37 genes. These genes might seem insignificant, but they’re crucial for the core function of mitochondria: creating cellular energy through oxidative phosphorylation.
The Importance of Quantity
Mitochondrial DNA levels or the number of mtDNA copies within a cell isn’t fixed. It varies depending on cell type, age, and even health conditions. Like muscle cells, cells with high energy demands typically have more mtDNA copies than those with lower needs. Interestingly, mitochondrial DNA levels also fluctuate throughout our lives. Studies suggest a decline in mtDNA copy number as we age, which may be linked to age-related diseases.
Changes in mtDNA abundance can reflect a reduced number of mitochondria or can be due to reduced genome copies within the mitochondria.
When Levels Go Awry
Abnormal mitochondrial DNA levels can be a red flag. Mutations in mtDNA, or a significant decrease in its copy number, have been associated with various mitochondrial diseases. These can affect different body parts, causing symptoms like muscle weakness, vision problems, and even neurological disorders.
How Genetics May Influence Mitochondrial DNA Levels
The regulation of mitochondrial DNA levels is a pivotal aspect of cellular function, influencing overall wellness. In a recent study involving a substantial cohort from the UK Biobank, specific genes in non-mitochondrial DNA were pinpointed as influencers of mtDNA abundance in the blood. Below are some of these genes, categorized by function. Certain genetic variants (SNPs) in all of these genes were associated with variation in mtDNA levels and some are highlighted below:
Immune System Modulators
- CXCL6: This gene, encoding a chemokine, may influence mitochondrial DNA levels through its role in immune response and inflammation. Immune system activation or modulation can impact cellular processes, potentially affecting mtDNA abundance.
- MEF2C is known for its involvement in immune system regulation and muscle development. SNP rs114694170 inMEF2C was found to contribute to variations in mitochondrial DNA levels.
- ITPR3: As a gene in intracellular calcium signaling, ITPR3 may impact mitochondrial function by influencing calcium levels, which are crucial for mitochondrial processes.
- UBE2D1: This gene, involved in protein degradation, might influence mitochondrial DNA levels by regulating the turnover of proteins crucial for mitochondrial function and maintenance.
- STIM1, PNP, CRK, SIRPB1: These genes are associated with immune system functions and may indirectly affect mitochondrial DNA levels through their roles in immune response and cellular signaling. SNP rs1760940 in PNP is associated with elevated mtDNA levels
Cell Cycle and Cancer Regulators
- TERT: Telomerase activity, regulated by TERT, is linked to cellular lifespan. Altered TERT activity may impact cell division and mtDNA replication, influencing overall mitochondrial DNA levels.
- BAK1, CDK6, CDK10, SUFU, FANCI, MDFIC, JMJD1C, USP7, BIK: These genes are involved in apoptosis, cell cycle regulation, and DNA repair. Dysregulation of these processes can affect cellular health and influence mtDNA abundance. SNPs rs210143 in BAK1 and rs77236693 in MDFIC were found to be associated with mtDNA levels.
Mitochondrial Function Regulators
- MFN2: Critical for mitochondrial fusion, MFN2 may impact the overall mitochondrial network and mtDNA maintenance.
- TFAM: A key player in mitochondrial DNA replication and maintenance, variations in TFAM levels can directly affect mtDNA abundance. SNP rs11006132 in TFAM is associated with elevated mtDNA levels.
- DGUOK: This gene is involved in mitochondrial DNA synthesis, and changes in its activity can impact mitochondrial DNA levels.
- USP30: Associated with mitochondrial quality control and turnover, USP30’s functions can influence the overall abundance of mtDNA.
- CREB5: A transcription factor associated with mitochondrial function and energy metabolism, CREB5 plays a role in regulating mitochondrial DNA levels.
- POLG: Responsible for replicating mitochondrial DNA, variations in POLG activity can directly impact mtDNA abundance.
Mitochondrial DNA SNPs
While mitochondrial DNA abundance displayed associations with haplogroups, the combinations of mtDNA SNPs, the study found similar and consistent effect sizes for the most common haplogroups in the UK Biobank. Importantly, the genetic makeup of the mitochondrial genome itself did not emerge as a major determinant of mtDNA abundance changes. This suggests that, despite genetic variations in mitochondrial haplogroups, other factors substantially govern the observed variations in mitochondrial DNA levels.
Heritability
The SNP-heritability of mtDNA abundance was estimated to be 8.3%, indicating a substantial role of inherited genetic variants in governing mitochondrial DNA levels.
In summary, several genes and their variants have been identified that play critical roles in immune response, cell cycle regulation, and mitochondrial function, collectively impacting mitochondrial DNA levels. This breakdown sheds light on the genetic landscape governing mitochondrial DNA abundance. As we unravel these genetic intricacies, there emerges a pathway for targeted investigations and potential interventions.
Non-Genetic Factors Influencing Mitochondrial DNA Levels
The same study from the UK Biobank has also identified specific non-genetic factors influencing mitochondrial DNA levels. These include sex, age, lifestyle, haplogroups, blood markers, and biochemistry markers, shedding light on the multifaceted regulation of this essential cellular component.
Sex and Age
The study revealed notable associations between sex, age, and mitochondrial DNA abundance. Male sex exhibited a consistent decrease in mtDNA abundance, pointing towards a sex-specific influence on mitochondrial dynamics. Furthermore, advancing age was strongly correlated with reduced mtDNA abundance, indicating a progressive decline over the aging process. Intriguingly, menopausal status in women added another layer to this relationship, with age affecting mtDNA abundance differently in pre and post-menopausal women. This nuanced understanding underscores the importance of considering gender-specific and age-related factors in regulating mitochondrial DNA levels.
Lifestyle Factors
Lifestyle factors emerged as significant contributors to variations in mtDNA abundance. Both increased pack years, indicative of smoking exposure, and elevated BMI were negatively associated with mtDNA abundance in both men and women. The detrimental impact of smoking and higher BMI on mitochondrial DNA levels suggests potential links between these lifestyle factors and mitochondrial health. Notably, individuals with higher mtDNA abundance experienced better and longer survival, highlighting the potential long-term implications of lifestyle choices on mtDNA dynamics.
Blood Markers
The analysis extended to blood markers, revealing intriguing associations with mtDNA abundance. White and red blood cell counts exhibited significant correlations, with white blood cell count negatively linked to mtDNA abundance. The negative association of red blood cell counts with mtDNA abundance suggests that multiple mechanisms beyond nucleated cell count contribute to the regulation of mitochondrial DNA levels. Additionally, specific blood cell types, such as neutrophils, eosinophils, basophils, and monocytes, showed negative associations with mtDNA abundance, providing further insights into the intricate relationship between hematological parameters and mitochondrial dynamics.
Biochemistry Markers
The association between mtDNA abundance and various biochemistry markers was also unveiled in the study. Markers related to inflammation, kidney function, liver function, cholesterol metabolism, ion homeostasis, vitamin D levels, and glucose metabolism displayed significant correlations with mtDNA abundance. Notably, these associations persisted even after adjusting for immune cell count, with some markers showing increased effect sizes. The findings emphasize the multi-faceted nature of factors influencing mtDNA abundance, extending beyond immune cell contributions to broader biochemical processes.
Investigating the determinants of mitochondrial DNA abundance provides a comprehensive view of the intricate interplay between genetic, lifestyle, and biochemical factors. This knowledge enhances our understanding of cellular dynamics. It opens avenues for further research into targeted interventions for maintaining mitochondrial health and mitigating the impact of various factors on mtDNA abundance.
Conditions Related to Mitochondrial DNA Mutations
While common polymorphisms (SNPs) in nuclear DNA can affect mtDNA levels, rare mutations in the mitochondrial DNA itself can lead to a variety of diseases, affecting different parts of the body. Here’s a breakdown of some:
- Mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes (MELAS): This is a neurological disorder causing muscle weakness, recurrent strokes, headaches, and seizures.
- Leber hereditary optic neuropathy (LHON): This is a genetic condition leading to progressive vision loss, often starting in young adulthood.
- Kearns-Sayre syndrome (KSS): This syndrome affects multiple systems, causing progressive external ophthalmoplegia (drooping eyelids), heart problems, and muscle weakness.
- Myoclonic epilepsy with ragged red fibers (MERRF): This condition causes muscle weakness, seizures, and a characteristic muscle biopsy finding.
- Chronic progressive external ophthalmoplegia (CPEO): This condition leads to progressive weakness of the eye muscles, making it difficult to move the eyes.
- Mitochondrial diabetes and deafness (MERRF/MELAS overlap syndrome): This syndrome combines symptoms of MERRF and MELAS, including diabetes and hearing loss, as well as muscle weakness and seizures.
About the LifeDNA Wellness Report
Understanding even complex factors like those affecting Mitochondrial DNA Levels becomes pivotal as we navigate the intricate pathways of our wellness. Imagine having personalized insights into your unique genetic traits related to your well-being. This is where the LifeDNA Wellness Report steps in. Going beyond generic advice, this tool provides tailored recommendations based on your genetic code, offering a holistic perspective on your well-being. By unlocking your genetic insights, you can take proactive steps towards a brighter, more informed lifestyle with the LifeDNA Wellness Report. Get it today!
Summary
- Mitochondrial DNA (mtDNA) is a small yet crucial component within mitochondria, which powers cellular functions by converting food energy into ATP. Despite its size, mtDNA’s 37 genes play a pivotal role in cellular energy production through oxidative phosphorylation.
- Dynamic mtDNA levels vary by cell type, age, and health conditions. High-energy-demand cells possess more mtDNA copies, and studies indicate a decline in mtDNA copy number with age, potentially linked to age-related diseases.
- Abnormal mtDNA levels, marked by mutations or significant decreases, signal potential issues and may be associated with mitochondrial diseases, leading to symptoms like muscle weakness, vision problems, and neurological disorders.
- A recent UK Biobank study identified genes like CXCL6 and TERT that influence mtDNA levels through immune modulation, apoptosis, and telomerase activity, highlighting diverse genetic factors governing mtDNA abundance.
- The same study identified non-genetic factors like sex, age, lifestyle choices, blood markers, and biochemistry markers contributing to the intricate regulation of mtDNA abundance.
- Exploring the determinants of mitochondrial DNA abundance offers a comprehensive view of the interplay between genetic and non-genetic factors, enhancing our understanding of cellular dynamics and paving the way for targeted interventions in maintaining mitochondrial health.
References
*Understanding your genetics can offer valuable insights into your well-being, but it is not deterministic. Your traits can be influenced by the complex interplay involving nature, lifestyle, family history, and others.
Our reports and suggestions do not diagnose or treat any health conditions or provide any medical advice. Consult with a healthcare professional before making any major lifestyle changes or if you have any other concerns about your results.