Understanding the Genetics of ALA to EPA Conversion
Aira
on
August 16, 2024
What is ALA?
Alpha-lipoic acid (ALA), a potent antioxidant, plays a crucial role in cellular energy production and protection against oxidative stress. Also known as thioctic acid, ALA is a naturally occurring compound found in small amounts in certain foods and is also synthesized in the human body. Its unique feature lies in its ability to function in both water-soluble and fat-soluble environments, making it a versatile defender against free radicals.
ALA serves as a cofactor for various enzymes involved in energy metabolism, particularly within the mitochondria—the cell’s powerhouse. Scientific studies have underscored ALA’s potential in managing conditions associated with oxidative damage, such as diabetes and neurodegenerative disorders. Research suggests that ALA may enhance insulin sensitivity, offering promising implications for individuals with type 2 diabetes.
This antioxidant has also garnered attention for its neuroprotective properties, with studies indicating potential benefits in conditions like Alzheimer’s disease. Furthermore, ALA’s role in mitigating inflammation and supporting cardiovascular health adds to its multifaceted appeal. This process might also be particularly relevant to people with special diets like vegetarians.

Is ALA as Good as DHA and EPA?
While alpha-lipoic acid (ALA) shares antioxidant properties with docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA), they serve distinct roles in the body. DHA and EPA, omega-3 fatty acids predominantly found in fatty fish, are crucial components of cell membranes, particularly in the brain and retina. Scientific studies highlight their pivotal role in cognitive function, cardiovascular health, and modulation of inflammatory response.
ALA, on the other hand, functions primarily as an antioxidant and cofactor in cellular energy metabolism. While ALA contributes to overall cellular health, it doesn’t possess the same structural significance as DHA and EPA in neural tissues. Notably, the body can convert ALA into small amounts of DHA and EPA, but the conversion efficiency is limited.
What is EPA?
Eicosapentaenoic Acid (EPA) is a long-chain omega-3 fatty acid abundantly present in fatty fish, such as salmon, mackerel, and sardines. It belongs to the family of polyunsaturated fatty acids (PUFAs) and plays a critical role in human health. Scientific studies consistently underscore the importance of EPA in cardiovascular well-being, primarily due to its anti-inflammatory and anti-thrombotic properties.
EPA serves as a precursor to bioactive lipid mediators, namely resolvins and protectins, which actively participate in resolving inflammation and promoting tissue repair. Its ability to compete with arachidonic acid for enzymatic conversion leads to the production of eicosanoids with reduced inflammatory potential, contributing to the overall anti-inflammatory effects.
Research also suggests that EPA influences lipid metabolism, modulates blood lipid profiles, and exhibits favorable effects on blood pressure, collectively contributing to a cardioprotective role. Furthermore, EPA has demonstrated efficacy in the management of various inflammatory conditions, including rheumatoid arthritis.
As a fundamental component of cell membranes, particularly in the brain, EPA is implicated in cognitive function and mental health. The incorporation of EPA-rich foods or supplements into the diet is recognized as a valuable strategy to support cardiovascular and cognitive health, emphasizing its significance in maintaining overall well-being.
How Does ALA to EPA Conversion Work?
The conversion of Alpha-Lipoic Acid (ALA) to Eicosapentaenoic Acid (EPA) involves a series of enzymatic reactions within the human body. ALA is an omega-3 fatty acid, but it differs structurally from EPA. The conversion primarily occurs through a series of desaturation and elongation steps, catalyzed by various enzymes.
The initial step involves the desaturation of ALA by the enzyme delta-6 desaturase (coded by FADS2), leading to the formation of stearidonic acid (SDA). Subsequently, SDA undergoes further desaturation, facilitated by delta-5 desaturase (coded by FADS1), resulting in the production of eicosatetraenoic acid (ETA). Finally, elongation of ETA is mediated by elongase enzymes, ultimately yielding EPA.
While the body has the capacity to convert ALA to EPA, the efficiency of this process is limited. Various factors, including dietary composition, genetics, and overall health, influence the rate of conversion. It’s noteworthy that the conversion of ALA to EPA and its subsequent metabolites is generally less efficient than obtaining EPA directly from dietary sources, such as fatty fish or EPA-rich supplements. Therefore, for individuals seeking to increase EPA levels, direct consumption of EPA or DHA sources may be a more effective approach than relying solely on ALA conversion pathways.
What Affects ALA to EPA Conversion?
Several factors influence the conversion of Alpha-Lipoic Acid (ALA) to Eicosapentaenoic Acid (EPA) in the human body. From dietary considerations to genetic predispositions, understanding the determinants of this conversion is crucial for optimizing omega-3 fatty acid intake and reaping the associated health benefits.
Genetic Factors
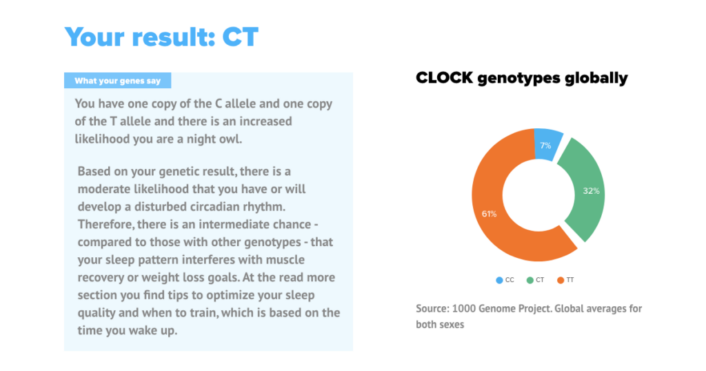
Genetics significantly influence the conversion of Alpha-Lipoic Acid (ALA) to Eicosapentaenoic Acid (EPA). Variations in key genes like FADS2 impact the efficiency of this conversion, shedding light on individual differences in omega-3 fatty acid metabolism and highlighting the role of genetics in dietary health.
FADS2
Genetic factors impact the levels of long-chain n-3 polyunsaturated fatty acids (PUFAs), derived from diet or via alpha-linolenic acid (ALA) conversion. In a study across five cohorts, variations in desaturase genes (FADS1, FADS2) were linked to ALA levels and inversely to levels of eicosapentaenoic acid (EPA) and docosapentaenoic acid (DPA). In addition, elongase gene (ELOVL2) variations were associated with higher EPA and DPA, and lower docosahexaenoic acid (DHA) levels. A novel association was also found between DPA and SNPs in GCKR.
The study suggests a reduced ALA-to-EPA conversion rate in subjects with specific FADS2 variations, such as rs1535. Similar trends were observed in various ethnicities. Understanding these genetic influences sheds light on how genes and the environment interact to affect in circulating essential fatty acid levels.
Environmental Factors
Several environmental factors can influence the conversion of Alpha-Lipoic Acid (ALA) to Eicosapentaenoic Acid (EPA) in the human body, affecting the efficiency of this critical process. Understanding these factors is essential for optimizing omega-3 fatty acid intake and reaping the associated health benefits.
- Dietary Composition: The type and amount of dietary fats play a pivotal role in ALA to EPA conversion. A diet rich in omega-3 fatty acids, particularly from marine sources like fatty fish (e.g., salmon, mackerel), provides direct access to EPA, bypassing the need for conversion. Conversely, diets high in omega-6 fatty acids, commonly found in vegetable oils, can compete with ALA for the same enzymes involved in the conversion process, potentially reducing the efficiency of ALA conversion to EPA.
- Nutrient Status: Adequate levels of certain nutrients are crucial for optimal conversion. For instance, the conversion of ALA to EPA involves various enzymes that require co-factors, including vitamins B3, B6, C, and the minerals zinc and magnesium. Insufficient levels of these nutrients may hinder the enzymatic reactions, impacting the efficiency of the conversion process.
- Oxidative Stress: Oxidative stress, resulting from an imbalance between free radicals and antioxidants, can interfere with the ALA to EPA conversion. Reactive oxygen species generated during oxidative stress may damage the enzymes involved in the conversion pathway, reducing their activity and impeding the overall process.
- Inflammation: Chronic inflammation has been linked to reduced efficiency in ALA conversion. Inflammatory conditions can alter the expression of key enzymes involved in the conversion process, disrupting the delicate balance required for optimal omega-3 metabolism.
- Age and Gender: Age and gender can also affect conversion efficiency. Studies have suggested that the conversion rate may be significantly higher in women of reproductive age compared to men and postmenopausal women. Additionally, aging may lead to a decline in enzymatic activity, potentially reducing the conversion efficiency in older individuals.
- Health Conditions: Certain health conditions, such as diabetes and metabolic syndrome, have been associated with impaired ALA to EPA conversion. These conditions may alter the expression and activity of enzymes involved in the pathway, influencing the overall effectiveness of the conversion process.
Understanding the interplay of these environmental factors together with the genetic predisposition is crucial for individuals seeking to optimize their omega-3 fatty acid status. A holistic approach, encompassing dietary choices, nutrient intake, and lifestyle factors, can contribute to enhancing the efficiency of ALA to EPA conversion and, consequently, reaping the full spectrum of health benefits associated with omega-3 fatty acids.
Why are Omega-3 Fatty Acids Important to the Body?
Omega-3 fatty acids, especially the EPA and DHA, are essential components crucial for maintaining optimal health. Scientific evidence underscores their importance in various physiological processes:
- Cardiovascular Health: EPA and DHA contribute to cardiovascular health by reducing triglyceride levels, lowering blood pressure, and inhibiting platelet aggregation. These actions collectively mitigate the risk of cardiovascular diseases.
- Brain Function and Development: DHA, particularly abundant in the brain, is essential for neurodevelopment in infants and supports cognitive function throughout life. Studies suggest that omega-3 fatty acids may play a role in reducing the risk of neurodegenerative disorders.
- Inflammation Regulation: EPA and DHA possess anti-inflammatory properties, influencing the production of inflammatory mediators. This anti-inflammatory effect is crucial in managing chronic inflammatory conditions and promoting overall immune system balance.
- Eye Health: DHA is a key component of the retina, and adequate levels are associated with a lower risk of age-related macular degeneration (AMD). Omega-3s contribute to maintaining visual acuity and protecting ocular tissues.
- Joint Health: Omega-3 fatty acids exhibit anti-inflammatory effects that can be beneficial for individuals with joint disorders like rheumatoid arthritis. They may help alleviate symptoms and improve joint function.
- Mood and Mental Health: EPA and DHA play roles in neurotransmitter function and membrane fluidity in nerve cells. Research suggests that omega-3 supplementation may have antidepressant and mood-stabilizing effects, impacting mental health positively.
- Skin Health: Omega-3s contribute to skin health by promoting hydration, reducing inflammation, and supporting the skin barrier function. These factors collectively contribute to maintaining healthy skin.
- Reproductive Health: Omega-3 fatty acids are vital for reproductive health, influencing fertility, pregnancy, and lactation. DHA, in particular, is crucial for the development of the fetal nervous system.
- Metabolic Health: Omega-3 fatty acids may play a role in metabolic health by improving insulin sensitivity, reducing inflammation associated with obesity, and managing metabolic syndrome.
- Cancer Prevention: While research is ongoing, some studies suggest that omega-3 fatty acids may have a protective effect against certain types of cancer. Their anti-inflammatory and antioxidant properties are believed to contribute to this potential benefit.
Given their diverse roles in fundamental biological processes, maintaining adequate levels of omega-3 fatty acids through a balanced diet or supplementation is integral for overall health and well-being.
Is Omega-3 Good for Your Kidneys?
Emerging evidence suggests that omega-3 fatty acids, particularly EPA and DHA, may confer benefits for kidney health. Chronic kidney disease (CKD) is characterized by inflammation, oxidative stress, and altered lipid metabolism, and omega-3s exhibit properties that may address these factors.
- Anti-Inflammatory Effects: Omega-3 fatty acids are known for their anti-inflammatory properties. In CKD, inflammation plays a pivotal role in disease progression. Omega-3s may help modulate inflammatory responses, potentially mitigating kidney damage.
- Blood Pressure Regulation: Hypertension is a common contributor to kidney disease. Omega-3s have been associated with blood pressure reduction, contributing to the overall management of hypertension and potentially slowing the progression of CKD.
- Reduced Proteinuria: Proteinuria, the presence of excess proteins in the urine, is a marker of kidney dysfunction. Studies suggest that omega-3 supplementation may reduce proteinuria, indicating a potential protective effect on kidney function.
- Antioxidant Properties: Oxidative stress is implicated in CKD pathogenesis. Omega-3 fatty acids possess antioxidant capabilities, scavenging free radicals and attenuating oxidative damage, which could be beneficial for preserving kidney function.
- Improvement in Lipid Profiles: Dyslipidemia often accompanies CKD. Omega-3s may positively influence lipid metabolism, leading to favorable changes in lipid profiles. This, in turn, may contribute to cardiovascular health in individuals with compromised kidney function.
While these findings suggest potential benefits, it’s crucial to note that research on omega-3s and kidney health is ongoing, and individual responses may vary. Moreover, individuals with CKD should consult healthcare professionals before incorporating omega-3 supplements, as high doses may not be suitable for everyone.
In conclusion, the anti-inflammatory, antioxidant, and blood pressure-regulating properties of omega-3 fatty acids position them as promising candidates for supporting kidney health, but further research is needed to establish clear guidelines for their use in CKD management.
What are Foods Rich in Omega-3 Fatty Acids?
Foods rich in omega-3 fatty acids are essential for maintaining optimal health, as these polyunsaturated fats offer various health benefits. The primary omega-3 fatty acids of interest are plant-based ALA, eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA), predominantly found in marine sources. Here are some scientifically-backed examples of foods rich in omega-3s:
- Fatty Fish: Fatty fish like salmon, mackerel, sardines, herring, and trout are exceptional sources of EPA and DHA. Consuming these fish provides direct access to these essential omega-3 fatty acids.
- Chia Seeds: Chia seeds are plant-based sources of alpha-linolenic acid (ALA), a precursor to EPA and DHA. These tiny seeds are versatile and can be added to various dishes for a nutrient boost.
- Flaxseeds: Flaxseeds are another plant-based option rich in ALA. Grinding flaxseeds enhances their digestibility, allowing for better absorption of ALA.
- Walnuts: Walnuts contain ALA and are a convenient and tasty addition to salads, and yogurt, or enjoyed as a snack.
- Canola Oil: Canola oil is a cooking oil that contains ALA. Its neutral flavor makes it suitable for various culinary applications.
- Edamame: Edamame, or young soybeans, is a plant-based source of ALA and can be included in salads, stir-fries, or enjoyed as a snack.
- Seaweed and Algae: Certain types of seaweed and algae-based supplements provide a vegetarian source of EPA and DHA, particularly beneficial for individuals following plant-based diets.
- Hemp Seeds: Hemp seeds offer a combination of essential nutrients, including ALA. They can be sprinkled on salads, and yogurt, or incorporated into smoothies.
- Brussels Sprouts: Brussels sprouts contain small amounts of ALA and can be a valuable addition to a balanced diet rich in vegetables.
- Eggs Enriched with Omega-3s: Some eggs are enriched with omega-3 fatty acids by feeding hens a diet high in omega-3-rich foods or supplements. These eggs can provide a source of DHA.
Incorporating a variety of these omega-3-rich foods into a well-balanced diet contributes to meeting recommended daily intake levels. However, for those with specific dietary restrictions or challenges in obtaining sufficient omega-3s from food alone, supplementation or fortified products may be considered after consulting with a healthcare professional.
How to Maintain Essential Fatty Acids (EFAs) in the Body
Maintaining optimal levels of Essential Fatty Acids (EFAs) in the body is crucial for overall health, as these fats play vital roles in various physiological processes. The two main types of EFAs are omega-3 and omega-6 fatty acids, and achieving a balance between them is key to promoting health and preventing chronic diseases. Here’s a detailed guide on how to maintain EFAs in the body:
- Balanced Diet: A well-rounded diet that includes a variety of foods rich in both omega-3 and omega-6 fatty acids is fundamental. Incorporate fatty fish such as salmon, mackerel, and sardines for omega-3s, and sources like nuts, seeds, and vegetable oils for omega-6s.
- Limiting Processed Foods: Processed foods often contain oils high in omega-6 fatty acids, contributing to an imbalance in the omega-3 to omega-6 ratio. Minimizing the intake of processed and fried foods helps maintain a more favorable balance.
- Cooking with Olive Oil: Olive oil, particularly extra virgin olive oil, is rich in monounsaturated fats and contains a reasonable amount of omega-6 fatty acids. Olive oil for cooking and salad dressings can contribute to a balanced EFA profile.
- Choosing Lean Meats: Opting for lean cuts of meat and poultry helps reduce saturated fat intake and promotes a healthier balance of fatty acids.
- Avoiding Trans Fats: Trans fats, often found in partially hydrogenated oils, should be avoided. These unhealthy fats not only disrupt EFA balance but also contribute to cardiovascular risk.
- Supplementation: In some cases, dietary supplementation may be necessary, especially for individuals with specific dietary restrictions or health conditions. Omega-3 supplements, derived from fish oil or algae-based sources, can help ensure an adequate intake of EPA and DHA.
- Limiting Alcohol Intake: Excessive alcohol consumption can impair the body’s ability to convert ALA (omega-3) into the more bioactive forms of EPA and DHA. Moderating alcohol intake supports optimal EFA metabolism.
- Managing Stress: Chronic stress can impact the metabolism of EFAs and contribute to inflammation. Implementing stress-management strategies, such as mindfulness and exercise, supports overall EFA balance.
- Regular Monitoring and Professional Guidance: Regular health check-ups and consultation with healthcare professionals, including registered dietitians, can help assess EFA levels and provide personalized recommendations based on individual health needs.
Maintaining a balanced intake of omega-3 and omega-6 fatty acids is a dynamic process influenced by dietary choices and lifestyle factors. Striving for a diverse and nutrient-rich diet while being mindful of the sources and proportions of EFAs contributes to optimal health and wellness.
LifeDNA’s ALA to EPA Conversion Report
LifeDNA’s scientifically-backed Nutrition Report delves into your genetic makeup to provide personalized insights on how your body processes alpha-lipoic acid (ALA) into eicosapentaenoic acid (EPA).
Take control of your wellness journey by understanding your unique nutritional needs. Explore additional reports like the Saturated Fat Metabolism Report, Carbohydrate Metabolism Report, and Preference to Fatty Foods Report to gain a comprehensive understanding of your genetic predispositions.
Empower yourself with knowledge and make informed choices. Start your wellness journey today by subscribing to LifeDNA and unveiling the roadmap to a healthier, more vibrant you. Your genetic potential awaits — Try life DNA today.
Summary
- Plant-based Alpha-lipoic acid (ALA) is a potent antioxidant crucial for cellular energy production and defense against oxidative stress.
- ALA, DHA, and EPA share antioxidant properties but have distinct roles.
- DHA and EPA, abundant in fatty fish, are vital for cell membranes, cognitive function, and cardiovascular health.
- ALA primarily acts as an antioxidant and cofactor, with limited structural significance in neural tissues.
- Eicosapentaenoic Acid (EPA) is a long-chain omega-3 fatty acid crucial for cardiovascular health.
- ALA converts to EPA through desaturation and elongation steps catalyzed by enzymes. Initial desaturation produces stearidonic acid, followed by further desaturation leading to eicosatetraenoic acid. Elongation of eicosatetraenoic acid results in the formation of EPA, although conversion efficiency is limited.
- Variations in genes like FADS2 impact the conversion efficiency. Dietary composition, nutrient status, oxidative stress, inflammation, age, gender, and health conditions also influence this conversion.
- EPA and DHA are essential for cardiovascular health, brain function, inflammation regulation, eye health, joint health, mood, skin health, reproductive health, metabolic health, and potential cancer prevention.
- Fatty fish, chia seeds, flaxseeds, walnuts, canola oil, edamame, seaweed, algae, hemp seeds, Brussels sprouts, and omega-3-enriched eggs are scientifically-backed sources for the various Omega-3 fatty acids.
References
- https://www.webmd.com/diet/alpha-lipoic-acid-ala
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7423769/#:~:text=Energy%20metabolism%20is%20the%20process,multiple%20pathways%20to%20produce%20energy.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9824456/
- https://pubmed.ncbi.nlm.nih.gov/17982894/
- https://www.webmd.com/vitamins/ai/ingredientmono-864/docosahexaenoic-acid-dha
- https://www.webmd.com/vitamins/ai/ingredientmono-994/eicosapentaenoic-acid-epa
- https://www.heart.org/en/healthy-living/healthy-eating/eat-smart/fats/polyunsaturated-fats
- https://pubmed.ncbi.nlm.nih.gov/17343773/
- https://www.nutraingredients-usa.com/Article/2010/11/08/Omega-3-ALA-intakes-enough-for-EPA-DPA-levels-for-non-fish-eaters#
- https://journals.plos.org/plosgenetics/article?id=10.1371/journal.pgen.1002193
- https://lpi.oregonstate.edu/mic/other-nutrients/essential-fatty-acids
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9641984/#:~:text=Ingestion%20of%20omega%2D3%20fatty,tolerated%2C%20and%20risk%2Dfree.
- https://stanfordhealthcare.org/medical-clinics/cancer-nutrition-services/reducing-cancer-risk/omega-3-fatty-acids.html#:~:text=Researchers%20are%20studying%20the%20effects,Alpha%2Dlinolenic%20acid
- https://www.bmj.com/company/newsroom/omega-3-fatty-acids-in-seafood-linked-to-lower-risk-of-chronic-kidney-problems/#:~:text=Higher%20levels%20of%20omega%203,derived%20omega%203%20fatty%20acids.
- https://ods.od.nih.gov/factsheets/Omega3FattyAcids-Consumer/#:~:text=Fish%20and%20other%20seafood%20(especially,soybean%20oil%2C%20and%20canola%20oil)
- https://www.medicalnewstoday.com/articles/essential-fatty-acids#summary
*Understanding your genetics can offer valuable insights into your well-being, but it is not deterministic. Your traits can be influenced by the complex interplay involving nature, lifestyle, family history, and others.
Our reports have not been evaluated by the Food and Drug Administration. The contents on our website and our reports are for informational purposes only, and are not intended to diagnose any medical condition, replace the advice of a healthcare professional, or provide any medical advice, diagnosis, or treatment. Consult with a healthcare professional before making any major lifestyle changes or if you have any other concerns about your results. The testimonials featured may have used more than one LifeDNA or LifeDNA vendors’ product or reports.