Decoding the MTHFR Gene: What It Means for Your Wellness
Aira
on
August 16, 2024
What Is The MTHFR Gene?
The MTHFR gene, short for Methylenetetrahydrofolate Reductase, is crucial in the body’s metabolic processes. This gene is responsible for producing the MTHFR enzyme, which plays a vital role in processing amino acids, the building blocks of all proteins.
Specifically, MTHFR is a key in converting homocysteine, a potentially harmful amino acid, into methionine, a valuable and necessary amino acid. This process is essential for DNA methylation, which regulates gene expression and synthesizes DNA and RNA. Variations in the MTHFR gene can lead to reduced enzyme activity, affecting these critical metabolic processes.
This gene is also significant in folate (vitamin B9) metabolism, a vital nutrient for cell division and growth. It is actually crucial for various health conditions, including cardiovascular diseases and congenital disabilities.
Which Aspects Of Your Health Can The MTHFR Gene Influence?
The MTHFR protein plays a significant role in several aspects of health, primarily due to its involvement in processing amino acids and influencing folate metabolism. Here are some key health aspects influenced by the MTHFR:
Homocysteine Levels
MTHFR is crucial in converting homocysteine, a harmful amino acid, into methionine. Genetic variation in the MTHFR gene can lead to elevated homocysteine levels in the blood, a condition known as hyperhomocysteinemia.
A 2010 study showed that MTHFR C677T polymorphism accounted for 1.6% of the variation in homocysteine levels. High homocysteine levels are associated with an increased risk of cardiovascular issues like heart disease and stroke.
Folate Metabolism
The MTHFR enzyme plays a vital role in converting 5,10-methylenetetrahydrofolate to 5-methyltetrahydrofolate, a form of folate used in the methylation cycle. Variations in the MTHFR gene can affect the body’s ability to process folate (vitamin B9), leading to potential deficiencies.
Pregnancy and Fetal Development
Adequate folate levels are crucial for DNA synthesis and repair, making the MTHFR gene vital for pregnancy and fetal development. Genetic variation in this gene can increase the risk of complications such as neural tube defects in the fetus.
Response to Certain Medications
MTHFR status can influence how the body responds to certain medications, especially those affecting folate metabolism. It includes certain chemotherapy drugs.
It’s important to note that having these certain variants of the MTHFR gene doesn’t always cause health problems. The manifestation of health issues depends on various factors, including lifestyle, environmental exposures, and other genetic factors. Consulting with a healthcare provider for personalized advice and genetic counseling is advisable for those concerned about MTHFR’s possible mutations.
What is an MTHFR Gene Variation?
MTHFR gene variation refers to DNA sequence base changes in the MTHFR gene that can affect the function of the MTHFR enzyme. These variations can lead to elevated levels of homocysteine in the blood, known as hyperhomocysteinemia. This condition is associated with various health issues, including an increased risk of heart disease, stroke, and complications during pregnancy.
What are the Two Main MTHFR Gene Variations?
The two main variations (also called mutations) in the MTHFR (methylenetetrahydrofolate reductase) gene are C677T and A1298C.
MTHFR C677T (rs1801133 C>T, or G>A)
This variation is at base pair position 677 of the MTHFR gene. A change from cytosine (C) to thymine (T) can affect the enzyme’s function. People with two C677T (C to T) variants (one from each parent) have a homozygous mutation, which can lead to lower enzyme activity compared to those with no T or just one T-allele
- MTHFR 677 CC (two copies of C, one from each parent)
- MTHFR 677 CT (C from mother, T from father)
- MTHFR 677 TT (two copies of T, one from each parent).
This reduced activity can affect processes like folate metabolism and homocysteine levels in the body.
MTHFR A1298C (rs1801131 A>C, or T>G)
This base change occurs at position 1298 of the MTHFR gene, where cytosine (C) replaces adenine (A). Like C677T, individuals can be heterozygous (one copy of the C-allele variant) or homozygous (two copies of C) for this variant. The A1298C polymorphism can also impact the function of the MTHFR enzyme, but its effects are generally considered less severe than C677T.
These variations can impact the body’s ability to process folate and homocysteine, potentially leading to various health issues. However, the extent of their impact on health can vary among individuals, and having these variations does not necessarily mean that you will experience health problems.
It is better to consult with a healthcare provider for personalized advice and genetic counseling if there are concerns about MTHFR mutations.
Are MTHFR Gene Variations Clinically Significant?
MTHFR C677T
A 2016 study investigated the relationship between a specific genetic variation in the MTHFR gene (C677T) and the risk of breast cancer in North Indian women (275 cases and 275 controls). The research found a significant association between the CT genotype and the T allele of the MTHFR C677T variant and an increased genetic risk for breast cancer among this population.
A 2020 study investigated the impact of the MTHFR 677TT (two copies of the T-allele) genotype on blood pressure and hypertension risk. The study, drawing data from 6076 adults in the Joint Irish Nutrigenomics Organisation project, found that this genetic variant is associated with an increased risk of hypertension from 18 to 70 years of age. Additionally, the research revealed that low riboflavin (vitamin B2) status exacerbates this risk, particularly for those with the 677TT genotype. Those with the TT genotype also showed poorer blood pressure control when on antihypertensive treatment than those with the CT and CC genotypes.
A 2022 meta-analysis included 81 published studies and used odds ratios to assess the association between MTHFR genetic variations and susceptibility to psychiatric disorders. The results showed a significant link between the MTHFR C677T polymorphism and increased risks of schizophrenia, major depression, and bipolar disorder, particularly in the overall population and in specific ethnic groups (notably in Asian and African populations).
A significant association between the MTHFR C677T homozygous TT genotype and an increased risk of myocardial infarction in patients with diabetes mellitus was demonstrated in this 2023 study.
MTHFR A1298C
A 2016 meta-analysis found that the MTHFR A1298C polymorphism might contribute to an elevated risk of breast and ovarian cancer, particularly breast cancer among Caucasians.
How Do We Test for MTHFR Gene Variation?
Your DNA can be analyzed for the common MTHFR variations, C677T and A1298C. The test can be ordered by a healthcare provider, especially if there’s a history of conditions like recurrent miscarriages or blood clots or if a close family member has been diagnosed with an MTHFR variation. MTHFR test is also sometimes included as part of more comprehensive genetic testing panels.
Before undergoing the test, it’s essential to discuss with a healthcare provider the implications of the results and how they may affect overall health and treatment strategies. It’s important to understand that having an MTHFR variation doesn’t necessarily mean you will experience health problems related to that variation.
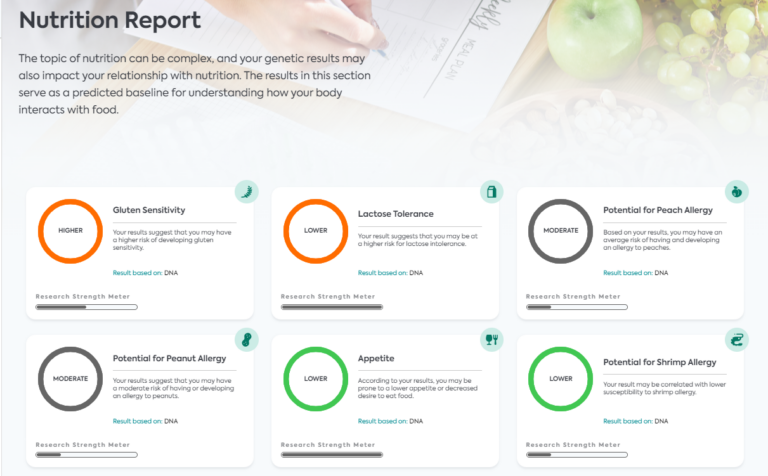
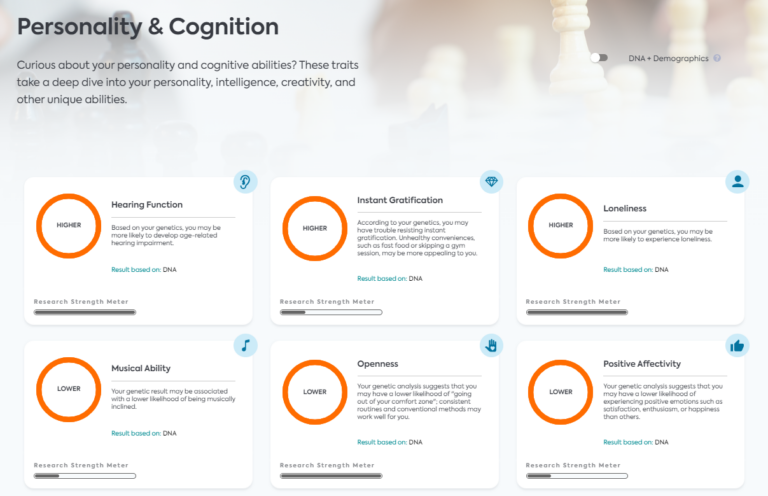
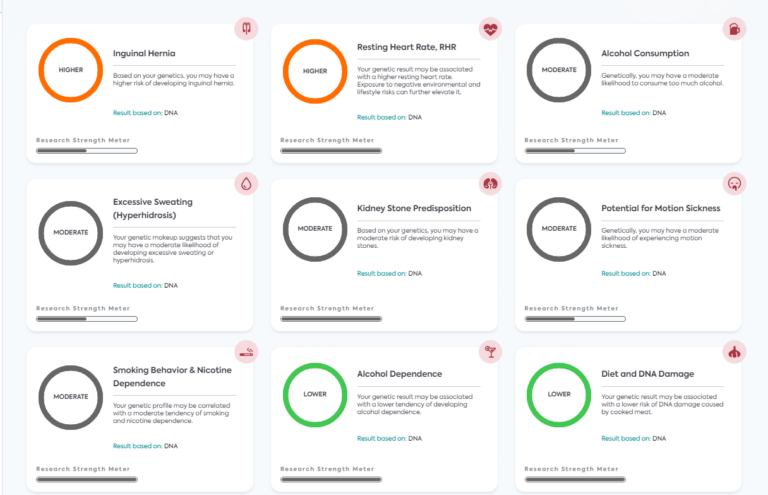
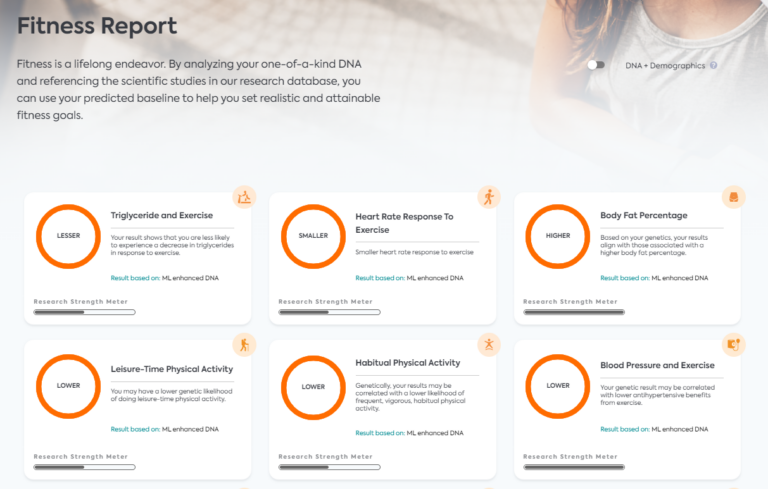
LifeDNA MTHFR Report
The LifeDNA MTHFR Report is a specialized genetic analysis focused on the MTHFR gene, which is well-known for its role in folate metabolism and many other health-related conditions. Our report provides individuals with detailed insights into their specific MTHFR gene variants and includes common polymorphisms like C677T and A1298C.
How Do You Manage Symptoms Caused by the MTHFR Gene Variation?
Treatment for the effects of MTHFR gene variation focuses on managing homocysteine levels and ensuring adequate folate intake. This can often be achieved through dietary changes and supplementation. Foods rich in natural folate include leafy greens, legumes, nuts, and fortified grains.
For individuals with elevated homocysteine levels or those who have difficulty metabolizing folic acid (the synthetic form of folate), healthcare providers may recommend supplements with L-methylfolate, the active form of folate.
Improving lifestyle factors like quitting smoking and controlling blood pressure can also help mitigate any associated risks. Working with a healthcare provider to determine the best approach is important, as treatment may vary based on individual health needs and other risk factors.
References
- https://medlineplus.gov/genetics/gene/mthfr/
- https://www.ncbi.nlm.nih.gov/books/NBK6561/
- https://www.ncbi.nlm.nih.gov/books/NBK66131/
- https://academic.oup.com/hmg/article/19/10/2050/699100
- https://www.webmd.com/heart-disease/homocysteine-risk
- https://www.cdc.gov/ncbddd/folicacid/mthfr-gene-and-folic-acid.html
- https://www.ncbi.nlm.nih.gov/books/NBK5968/
- https://pubmed.ncbi.nlm.nih.gov/32119295/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4499570/
- https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-020-01780-x
- https://www.frontiersin.org/articles/10.3389/fpsyt.2022.976428/full
- https://www.mdpi.com/2218-1989/13/2/251
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5416649/
- https://www.webmd.com/drugs/2/drug-162998/l-methylfolate-oral/details
*Understanding your genetics can offer valuable insights into your well-being, but it is not deterministic. Your traits can be influenced by the complex interplay involving nature, lifestyle, family history, and others.
Our reports have not been evaluated by the Food and Drug Administration. The contents on our website and our reports are for informational purposes only, and are not intended to diagnose any medical condition, replace the advice of a healthcare professional, or provide any medical advice, diagnosis, or treatment. Consult with a healthcare professional before making any major lifestyle changes or if you have any other concerns about your results. The testimonials featured may have used more than one LifeDNA or LifeDNA vendors’ product or reports.