
Have you ever wondered why some people seem to bounce back from falls effortlessly while others face the risk of fractures? It’s not just luck; it’s in your genes. Bone density refers to the amount of mineralized bone tissue in a given volume, serving as a critical indicator of skeletal strength and resilience. The density of bones is primarily influenced by the deposition of minerals like calcium and phosphorus within the bone matrix, forming a sturdy and rigid structure. This intricate balance is crucial for maintaining skeletal integrity and preventing fractures.
Quantitatively assessed through techniques such as dual-energy X-ray absorptiometry (DXA), bone density is expressed in grams per square centimeter. Peak bone density is typically achieved during early adulthood, but genetic factors play an important role in determining an individual’s baseline bone density. Specific genes regulate the development and turnover of bone tissue, impacting overall skeletal health.
Understanding the genetics of bone density is crucial in unraveling the mechanisms behind conditions like osteoporosis, where bone density decreases, leading to increased fracture susceptibility. As research delves deeper into the intricate interplay of genetic factors influencing bone health, insights gained hold the promise of personalized interventions and preventive measures to mitigate the risks associated with low bone density and fractures.
You might also like: From Genes to Cardiovascular Health: Understanding Blood Pressure and Exercise
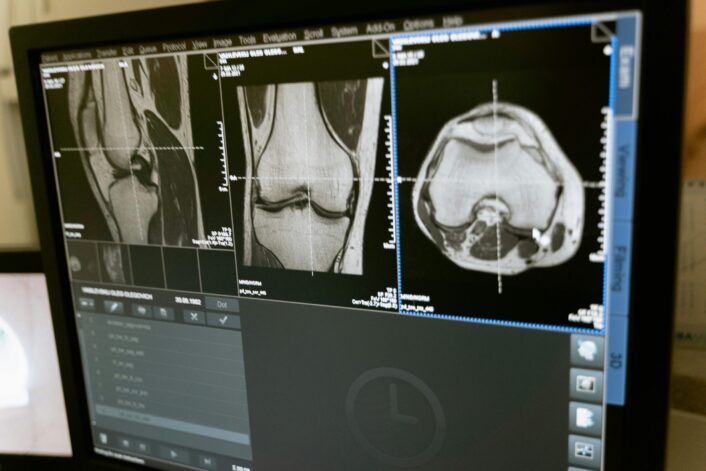
Fracture risk is the probability of sustaining a bone fracture, a multifactorial outcome influenced by various biological, environmental, and genetic factors. Key determinants of fracture risk include bone density, bone quality, and the mechanical forces applied to the bone. Low bone mineral density (BMD), as measured by tools like dual-energy X-ray absorptiometry (DXA), is a well-established risk factor for fractures, especially in conditions like osteoporosis.
Apart from BMD, bone quality encompasses factors such as microarchitecture, mineralization, and collagen composition. Integrating these elements is crucial for bone strength and fracture resistance. Age, sex, and lifestyle factors such as nutrition and physical activity also contribute significantly to fracture risk.
Accurate assessment and understanding of fracture risk are imperative for preventive strategies and interventions, especially in aging populations where fractures pose significant health burdens. Incorporating genetic insights alongside traditional risk factors enhances the precision of fracture risk prediction models, paving the way for targeted approaches to fracture prevention and management.
The relationship between bone density and fracture risk is well-established, with lower bone mineral density (BMD) correlating strongly with increased susceptibility to fractures, particularly in weight-bearing bones.
The mechanical properties of bone are intricately linked to its density, and diminished density compromises structural integrity. Conditions such as osteoporosis, characterized by reduced BMD, significantly elevate fracture risk. Osteoporotic fractures, often occurring in the hip, spine, and wrist, are associated with increased morbidity and mortality, particularly in the elderly.
Genetics plays a crucial role in shaping an individual’s bone density. Variations in genes regulating bone formation, resorption, and mineralization contribute to inter-individual differences in BMD. Understanding the genetic basis of bone density not only elucidates the pathophysiology of conditions like osteoporosis but also allows for personalized risk assessments.
Maintaining optimal bone density is a complex interplay of genetics, nutrition, physical activity, and hormonal balance. Strategies aimed at preserving bone health involve lifestyle modifications, nutritional interventions, and, in some cases, pharmacological treatments. Integrating genetic insights into fracture risk assessments enhances the precision of preventive approaches, guiding tailored interventions to mitigate the impact of low bone density on fracture susceptibility.
Genetics plays a pivotal role, with numerous genes identified as influencers of bone density and fracture susceptibility. Polymorphisms in genes associated with bone metabolism, structure, and mineralization contribute to inter-individual variations in fracture risk.
In one particular study using UK Biobank data, genetic factors influencing bone mineral density (BMD) were explored in a very large group of people. Phenotypic data on 394,929 individuals revealed a total of 142,417 DNA variants associated with estimated heel BMD (eBMD), identifying 1,362 independent SNPs clustered into 899 genome loci. Notable loci include genes WNT16, RSPO3, CCDC170, ESR1, and SPTBN. SNPs in these genes showed genome-wide significant associations with eBMD.
A polygenic risk score (PRS) was developed, and one particular score called LASSO4 PRS demonstrated the highest correlation with eBMD. This score, based on 22,886 predictors, outperformed a PRS model from previous work. Combining the LASSO4 PRS with physiological covariates, a novel BMD Osteoporosis Genetic (BOG) risk score was created. The combined score exhibited a higher correlation with eBMD (0.496) than either LASSO4 or physiological covariates alone.
What are polygenic risk scores and why they are important?
Individuals with lower BOG scores had significantly lower eBMD, emphasizing its potential as a predictive tool. The BOG score also demonstrated an association with osteoporosis risk, indicating its utility in identifying individuals at heightened risk for bone-related issues. The study also suggests that understanding genetic factors, particularly using the BOG score, could enhance predictions of BMD and associated risks for personalized health management.
Environmental factors influence bone density and fracture risk, interacting with genetic and hormonal elements to shape skeletal health. Several key factors contribute to variations in bone density and fracture susceptibility, with lifestyle and environmental considerations playing significant roles.
Understanding the intricate interplay between genetic and environmental factors is essential for comprehensive fracture risk assessment. Implementing lifestyle modifications, ensuring proper nutrition, and minimizing exposure to detrimental environmental influences can collectively contribute to maintaining optimal bone density and reducing the likelihood of fractures.
Bone density is closely linked to weight changes, as the mechanical loading of bones influences their adaptation and density. Weight-bearing activities subject bones to stress, prompting bone-forming cells (osteoblasts) to deposit mineralized tissue, thereby increasing bone density. Conversely, weight loss or reduced mechanical loading, as seen in conditions like anorexia nervosa or prolonged bed rest, can lead to bone loss due to decreased osteoblastic activity and increased osteoclastic bone resorption.
Body weight serves as a surrogate marker for the mechanical forces experienced by bones during daily activities. Higher body weight generally correlates with greater bone mineral density (BMD) because the skeletal system adapts to support the increased load. However, excessive body weight, as seen in obesity, may not necessarily translate to improved bone health, as the relationship between bone density and adiposity is complex.
Understanding the dynamic interplay between weight changes and bone density is crucial for assessing skeletal health. Both inadequate and excessive weight can impact bone metabolism, highlighting the importance of maintaining a healthy weight through balanced nutrition and weight-bearing physical activity to optimize bone density and overall skeletal strength.
You might be interested in: How Your Genes Influence Weight Change
Fracture risk is assessed through a combination of clinical evaluation and quantitative measurements, primarily focusing on bone health parameters. The gold standard for assessing fracture risk is dual-energy X-ray absorptiometry (DXA), which measures bone mineral density (BMD). Lower BMD, indicative of reduced bone mass, is a well-established predictor of increased fracture risk, particularly in postmenopausal women and the elderly.
Clinical risk factors, such as age, sex, family history, and previous fracture history, are integral components of fracture risk assessment. Additionally, tools like the FRAX® algorithm combine clinical risk factors with BMD measurements to estimate the 10-year probability of major osteoporotic fractures.
Recent advancements include the integration of genetic markers associated with bone metabolism into risk assessment models, offering a more personalized approach. Understanding the intricate interplay between genetic, clinical, and BMD factors allows for a comprehensive evaluation of fracture risk, guiding preventive strategies and interventions tailored to an individual’s specific risk profile.
Decreasing bone density, often associated with conditions like osteoporosis, may not manifest noticeable symptoms until fractures occur. However, as bone density diminishes, subtle signs and symptoms may emerge:
Bone density loss is often asymptomatic until fractures occur. Early detection through bone mineral density testing is crucial for assessing skeletal health and initiating preventive measures. Regular monitoring and appropriate interventions, including lifestyle modifications and pharmacological treatments, can mitigate the impact of decreased bone density and reduce the risk of fractures. Individuals experiencing these symptoms, especially those with risk factors, should consult healthcare professionals for timely evaluation and intervention.
Certain populations are more susceptible to fractures due to low bone density, with various risk factors contributing to this increased vulnerability.
Identifying individuals at risk for fractures due to low bone density is crucial for preventive strategies. Regular screening, lifestyle modifications, and, in some cases, pharmacological interventions can help mitigate the impact of decreased bone density and reduce the likelihood of fractures in these high-risk populations. Consulting healthcare professionals for personalized assessments and interventions is essential for optimizing skeletal health.
Optimizing bone density and reducing fracture risk involves a multifaceted approach that combines lifestyle modifications, nutritional interventions, and, in some cases, medical treatments. Here are evidence-based strategies:
Individuals should consult healthcare professionals for personalized advice based on their risk factors and health status. Implementing a comprehensive approach that addresses lifestyle, nutrition, and potential medical interventions is crucial for optimizing bone density and reducing the risk of fractures throughout the lifespan.
Know more about your bone health with LifeDNA’s Bone Density and Fracture Risk Trait Report. Our comprehensive genetic analysis delves deep into your unique genetic profile, providing valuable insights into factors influencing bone density and fracture susceptibility. Backed by rigorous scientific research, this report empowers you to take proactive steps toward optimizing your skeletal health.
Understanding your genetic predispositions is a game-changer in the pursuit of overall wellness. LifeDNA’s Fitness Report suite goes beyond bone health, offering reports on traits such as Aerobic Capacity, Power vs. Endurance, and Weight Loss and Exercise. With seven main categories and nearly 200 trait reports under Fitness, Wellness, Nutrition, Vitamins and Supplements, Sleep, and Personality and Cognition, our platform tailors recommendations based on your genetic makeup.
Embark on a transformative wellness journey by exploring LifeDNA’s diverse range of reports. Discover how your body responds to exercise, uncover dietary preferences, and gain insights into sleep patterns. Our subscription packages offer access to a wealth of genetic information, empowering you to make informed lifestyle choices.
Invest in your well-being today and seize the opportunity to optimize your fitness, nutrition, and overall health. Avail of LifeDNA’s subscriptions and embark on a personalized journey towards a healthier and happier you. Your genetic roadmap awaits – take the first step towards a life of wellness with LifeDNA.
*Understanding your genetics can offer valuable insights into your well-being, but it is not deterministic. Your traits can be influenced by the complex interplay involving nature, lifestyle, family history, and others.
Our reports have not been evaluated by the Food and Drug Administration. The contents on our website and our reports are for informational purposes only, and are not intended to diagnose any medical condition, replace the advice of a healthcare professional, or provide any medical advice, diagnosis, or treatment. Consult with a healthcare professional before making any major lifestyle changes or if you have any other concerns about your results. The testimonials featured may have used more than one LifeDNA or LifeDNA vendors’ product or reports.


