Does Genetics Dictate Your Vitamin E Levels?
Aira
on
February 8, 2024
What is Vitamin E?
Vitamin E, a fat-soluble vitamin vital for numerous bodily functions, is a powerful protector against free radicals. Our metabolism and environmental factors like smoke and radiation produce these harmful molecules. Unlike a physical shield, Vitamin E works behind the scenes, neutralizing these free radicals before they can damage our cells.
Beyond this crucial defense, Vitamin E plays a key role in maintaining healthy vision, reproduction, and the function of our blood, brain, and skin. Research suggests it may even contribute to managing metabolic disorders like obesity, diabetes, hypertension, and dyslipidemia.
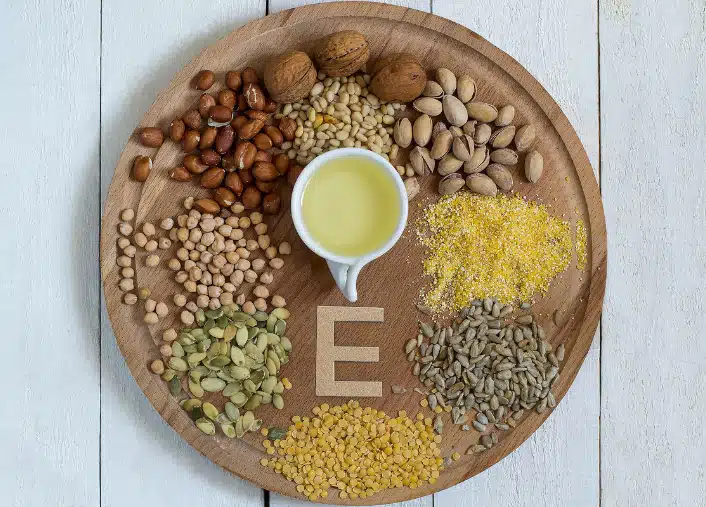
Luckily, obtaining this essential vitamin is easy. Vitamin E is abundant in various foods, including vegetable oils (corn, cottonseed, soybean, safflower), wheat germ, whole-grain cereals, and leafy green vegetables. While cooking and storage can reduce its presence, a balanced diet ensures we receive adequate amounts.

Importance of Vitamin E
Vitamin E is of great importance to our health due to its various roles:
- Antioxidant Properties: Vitamin E is a potent antioxidant that helps protect your cells against the effects of free radicals. Free radicals are molecules produced when your body breaks down food or is exposed to harmful environmental factors like tobacco smoke and radiation. They might play a role in heart disease, cancer, and other diseases.
- Cell Function and Protection: Vitamin E is crucial for the proper function of many organs in the body. It protects the cells of the body from damage by harmful free radicals.
- Metabolic Processes: Vitamin E may benefit various metabolic disorders, such as obesity, diabetes, hypertension, and dyslipidemia.
- Nervous System: Vitamin E is essential for the proper function of nerves and muscles. It acts as a protective antioxidant for nerve cells, helping to prevent oxidative damage. This is crucial for maintaining the integrity of the nervous system, including the transmission of nerve signals and the overall health of neurons. Adequate levels of vitamin E contribute to maintaining nerve cell membranes, which is vital for their proper function.
- Reproductive Health: Vitamin E plays a significant role in reproductive health. It is involved in the development of both male and female reproductive systems. In males, vitamin E is crucial for the health of sperm cells and their ability to fertilize an egg. In females, it supports the health of the uterus and may play a role in fertility. Vitamin E’s antioxidant properties help protect reproductive cells from damage caused by free radicals, which is important for overall reproductive function.
- Skin Health: Vitamin E is renowned for its contributions to skin health. As an antioxidant, it helps protect the skin from the damaging effects of free radicals induced by exposure to ultraviolet (UV) rays and environmental pollutants. Vitamin E also supports the production of collagen, a protein essential for maintaining skin elasticity and preventing premature aging. Including vitamin E in skincare routines or through dietary sources can contribute to a healthier complexion.
- Vision: Vitamin E is crucial for maintaining good vision. It plays a role in preventing age-related macular degeneration (AMD), a condition that can lead to vision loss. As an antioxidant, vitamin E helps protect the cells in the eyes from oxidative damage. Additionally, it may contribute to the prevention of cataracts, another common eye condition associated with aging. Ensuring adequate vitamin E intake is thus important for promoting long-term eye health.
- Immune System: Vitamin E is vital for maintaining a healthy immune system. It enhances the activity of immune cells, such as T cells and macrophages, which play key roles in defending the body against infections. The antioxidant properties of vitamin E also contribute to immune health by neutralizing free radicals that can compromise the immune response. Ensuring sufficient levels of vitamin E is important for overall immune function and resilience against infections.
- Brain Function: Vitamin E contributes to healthy brain function. It is believed to protect brain cells from oxidative stress, which is implicated in neurodegenerative diseases. While research on vitamin E and cognitive function is ongoing, some studies suggest that it may have a role in reducing the risk of cognitive decline associated with aging. However, the relationship between vitamin E and brain health is complex, and more research is needed to fully understand its mechanisms and potential benefits.
It’s important to note that while vitamin E plays these roles in the body, individual responses may vary, and it’s always advisable to consult with healthcare professionals for personalized advice on vitamin E supplementation or dietary adjustments.
Genetics of Vitamin E Levels
Genetic variations play a significant role in determining individual vitamin E levels. These variations affect how our bodies absorb, transport, and utilize this crucial antioxidant. Understanding these genetic influences can revolutionize our approach to optimizing vitamin E levels, paving the way for personalized strategies and improved health outcomes.
BUD13, ZNF259(ZPR1), and APOA1/C3/A4/A5
The genetic variant rs964184, located on chromosome 11q23.3, has been associated with alpha-tocopherol levels. This locus is situated in a gene-rich region at gene ZNF259(ZPR1) and between gene BUD13, and the gene cluster APOA1/C3/A4/A5.
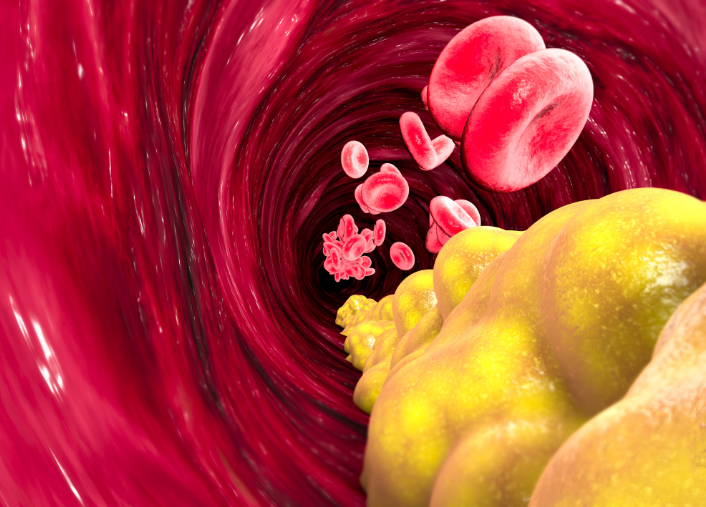
APOA1/C3/A4/A5 is known for its involvement in lipid metabolism and regulation. The presence of this SNP suggests a potential link between vitamin E levels and processes related to lipid metabolism.
Close to the BUD13 there is also another significant SNP for Vitamin E levels, rs12272004.
The replicated findings in this meta-analysis strengthen the found associations, emphasizing the significance of these genetic markers in influencing alpha-tocopherol concentrations. Further research may uncover the precise mechanisms by which these genes contribute to vitamin E regulation.
SCARB1
The genetic variant rs11057830, located on chromosome 12q24.31, represents another locus associated with alpha-tocopherol levels. This locus is situated near the SCARB1 gene, which plays a role in lipid metabolism and is involved in regulating cholesterol levels. Identifying this SNP suggests a potential connection between vitamin E levels and lipid-related processes mediated by SCARB1.
Exploring the specific interactions between SCARB1 and vitamin E metabolism may provide valuable insights into the regulatory pathways involved.
CYP4F2
The genetic variant rs2108622, located on chromosome 19pter-p13.11, is another novel SNP associated with alpha-tocopherol levels. This locus is situated near the CYP4F2 gene, known for its role in metabolizing various compounds, including vitamin E. The identification of this SNP suggests a potential impact on vitamin E metabolism, influencing its circulating levels.
In the meta-analysis, the association with CYP4F2 was reaffirmed, highlighting the importance of this genetic marker in the context of vitamin E regulation. Further investigations into the specific interactions between CYP4F2 and vitamin E metabolism could provide valuable insights into the underlying mechanisms.
These genetic variants identified through GWAS shed light on the intricate relationship between genetics and the response to long-term vitamin E supplementation, providing valuable insights into personalized approaches to nutritional interventions.
Non-Genetic Factors Influencing Vitamin E Levels
It’s important to know that genes alone do not influence vitamin E levels – several other factors do as well. Below are some insights on what other components interact with vitamin E concentrations within our body.
Nutritional Intake
Vitamin E is present in numerous food items, encompassing vegetables, fruits, meats, and animal products. Noteworthy sources include canola oil, olive oil, margarine, almonds, and peanuts.
Fat Absorption Mechanisms
As a fat-soluble vitamin, the absorption of vitamin E in the gastrointestinal tract is contingent upon processes governing fat absorption or metabolism. Consequently, individuals with conditions leading to fat malabsorption (e.g., Celiac disease, Crohn’s disease, pancreatic disorders) may experience a gradual deficiency in vitamin E over time.
Interaction with Other Nutrients
Deficiencies in iron and zinc can influence vitamin E metabolism and impede the transport of vitamin E stores from the liver to other body tissues.
Health Conditions
Various health conditions can impact vitamin E levels. For instance, metabolic disorders like obesity, diabetes, hypertension, and dyslipidemia may influence vitamin E concentrations.
Supplement Usage
The dosage of vitamin E in supplements is another contributing factor. In the United States, the median daily intake of vitamin E from food typically ranges from 5 to 10 milligrams (mg). Vitamin E supplements commonly provide concentrations of 268 or 537 mg (equivalent to 400 or 800 international units).
Understanding these factors can help individuals and healthcare providers develop strategies to maintain optimal Vitamin E levels. However, it’s important to consult with a healthcare provider for personalized advice.
Signs of Vitamin E Deficiency
Vitamin E deficiency can manifest in several ways:
- Muscle Weakness: Vitamin E is essential to the central nervous system. Its deficiency can result in oxidative stress, leading to muscle weakness.
- Coordination and Walking Difficulties: A deficiency can cause certain neurons, called the Purkinje neurons, to break down, harming their ability to transmit signals.
- Numbness and Tingling: Damage to nerve fibers can prevent the nerves from transmitting signals correctly, resulting in these sensations, also known as peripheral neuropathy.
- Vision Deterioration: A vitamin E deficiency can weaken light receptors in the retina and other cells in the eye. This can lead to loss of vision over time.
- Immune System Problems: Some research suggests a lack of vitamin E can inhibit the immune cells.
- Retinopathy and Dry Skin: These are also reported signs of Vitamin E deficiency.
Please consult with a healthcare provider if you experience any of these symptoms. They can conduct a blood test to determine your vitamin E levels.
Maintaining Adequate Vitamin E Levels
Maintaining adequate levels of Vitamin E in the body primarily involves dietary considerations and lifestyle habits. Here are some strategies:
- Dietary Intake: Consuming a balanced diet rich in Vitamin E is the most direct way to maintain adequate levels. Foods rich in Vitamin E include canola oil, olive oil, margarine, almonds, peanuts, meats, dairy, leafy greens, and fortified cereals.
- Supplements: Vitamin E is also available as an oral supplement in capsules or drops. However, it’s important to consult with a healthcare provider before starting any supplement regimen.
- Healthy Lifestyle: Regular exercise, adequate sleep, and a balanced diet can contribute to overall health and help maintain adequate levels of all vitamins, including Vitamin E.
- Regular Check-ups: Regular health check-ups can help monitor Vitamin E levels and detect any deficiencies early.
- Special Considerations: Certain health conditions, such as fat malabsorption disorders, can affect Vitamin E absorption. Individuals with these conditions may require specific dietary adjustments or supplements.
Remember, the recommended daily amount of Vitamin E for adults is 15 milligrams, and more is not necessarily better. The upper limit for adults is 1,000 mg/day for supplements.
Always consult with a healthcare provider for personalized advice. The LifeDNA Vitamins & Supplements Report may also help!
About the LifeDNA Vitamins and Supplements Report
For a more precise approach to your wellness, consider obtaining the LifeDNA Vitamins and Supplements Report today. This report provides specific insights with the Vitamin E Levels trait report, helping you understand how your body processes and utilizes this essential nutrient. By learning about the genetic factors affecting your vitamin E metabolism, you can make more informed decisions about your supplementation needs.
Take this opportunity to gain detailed information about your genetic predispositions now!
Summary
- Genetic variations significantly influence vitamin E levels, shaping absorption and utilization. Understanding these factors revolutionizes health strategies.
- Vitamin E defends against free radicals and supports vision, reproduction, skin health, and brain function. Research suggests benefits for metabolic disorders.
- Vitamin E acts as an antioxidant, supports cell function, and influences metabolic processes. It plays a vital role in various bodily functions.
- Genetic variants rs964184 and rs12272004 near lipid metabolism genes indicate a link between vitamin E levels and lipid processes.
- Variant rs11057830 near SCARB1 suggests a connection between vitamin E levels and lipid regulation.
- Variant rs2108622 near CYP4F2 impacts vitamin E metabolism, offering insights into additional regulatory mechanisms.
- Nutritional intake, fat absorption, nutrient interactions, health conditions, and supplement use influence vitamin E levels.
- Deficiency manifests through muscle weakness, coordination difficulties, numbness, vision deterioration, immune issues, and skin problems.
- A balanced diet, healthy lifestyle, regular check-ups, and supplements when needed contribute to optimal vitamin E levels. Consult healthcare providers for personalized advice.
References
- https://www.mayoclinic.org/drugs-supplements-vitamin-e/art-20364144
- https://pubmed.ncbi.nlm.nih.gov/26148343/
- https://www.mayoclinic.org/drugs-supplements/vitamin-e-oral-route/description/drg-20068918
- https://www.sciencedirect.com/science/article/pii/S0022316622028127?via%3Dihub
- https://academic.oup.com/hmg/article/20/19/3876/601498
- https://www.cdc.gov/nutritionreport/pdf/nr_ch2a.pdf
- https://newsnetwork.mayoclinic.org/discussion/possible-risks-associated-with-taking-vitamin-e-supplements/
- https://ods.od.nih.gov/factsheets/VitaminE-Consumer/
*Understanding your genetics can offer valuable insights into your well-being, but it is not deterministic. Your traits can be influenced by the complex interplay involving nature, lifestyle, family history, and others.
Our reports have not been evaluated by the Food and Drug Administration. The contents on our website and our reports are for informational purposes only, and are not intended to diagnose any medical condition, replace the advice of a healthcare professional, or provide any medical advice, diagnosis, or treatment. Consult with a healthcare professional before making any major lifestyle changes or if you have any other concerns about your results. The testimonials featured may have used more than one LifeDNA or LifeDNA vendors’ product or reports.