Using Genetic Data to Manage your Cholesterol Levels
Renette Salvador
on
July 4, 2025
Disclaimer: This article is for informational purposes only and is not intended to diagnose any conditions. LifeDNA does not provide diagnostic services for any conditions mentioned in this or any other article.
What Is Cholesterol?
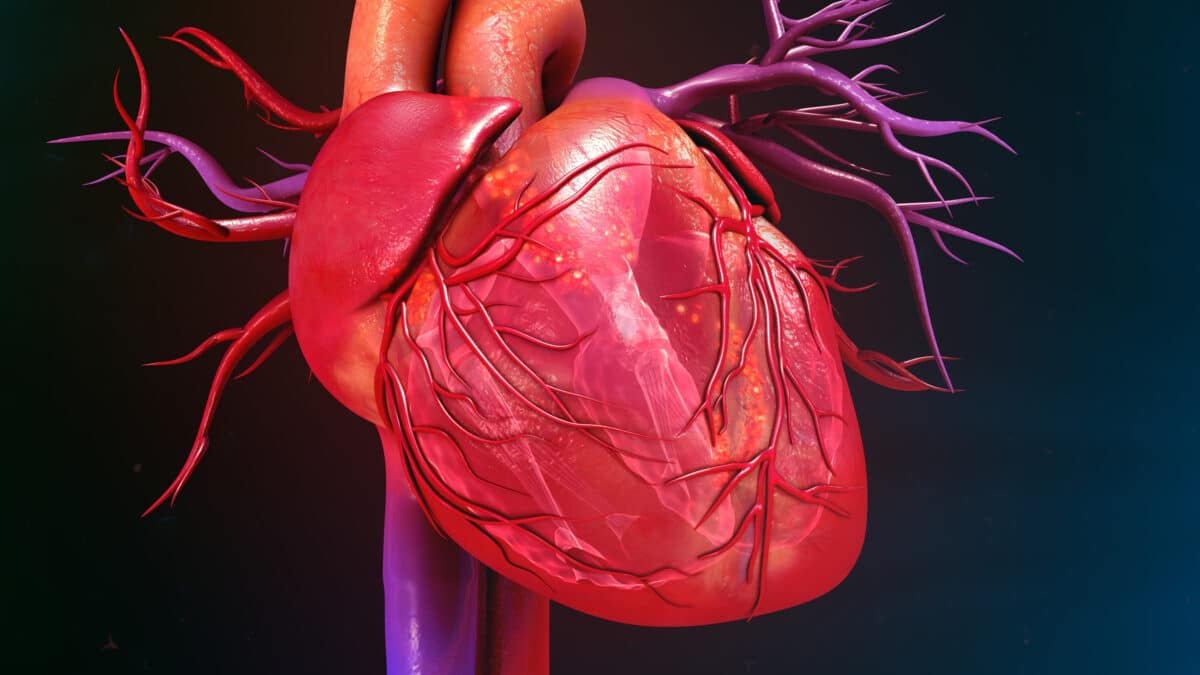
Cholesterol is a waxy, fat-like substance that your body needs to stay healthy. It helps build cells, make hormones, and produce vitamin D. Your body makes most of the cholesterol it needs in the liver, but you also get some from foods like meat, cheese, eggs, and butter. While cholesterol is important, having too much of it in your blood can be dangerous. When there’s an unhealthy amount of cholesterol, it may stick to the walls of your arteries. These are the blood vessels that carry oxygen-rich blood to your heart and other parts of your body.
You may want to read: How Can Genetics Influence Cholesterol Levels?
What Are The Two Types of Cholesterol?
There are two main types of cholesterol, and they have very different effects on your health. LDL, or low-density lipoprotein is often called the “bad” cholesterol. That’s because too much LDL can build up in your arteries forming a thick, hard substance called plaque. On the other hand, HDL, or high-density lipoprotein, is known as the “good” cholesterol. HDL helps remove extra cholesterol from your blood and carries it back to the liver, where your body can get rid of it.
Why Can Cholesterol Be a Problem?
Cholesterol is important for your body to function properly, but having too much of it, especially the wrong kind can be harmful. Cholesterol travels through your bloodstream, and when there is too much low-density lipoprotein (LDL), it can begin to stick to the walls of your arteries. Over time, this sticky buildup may narrow or block your arteries. When blood has a harder time flowing through your body, your heart has to work harder to keep things moving. This increases your risk of serious health problems, including heart disease. If an artery becomes completely blocked, it may lead to a heart attack or stroke. That’s why keeping your cholesterol levels in a healthy range is so important for your long-term heart and brain health.
What Affects Your Cholesterol Levels?
Your cholesterol levels are influenced by a mix of lifestyle choices and inherited traits. One of the biggest factors is your diet. Eating a lot of fried, fatty, or highly processed foods, like fast food, chips, and baked goods can increase the amount of LDL in your blood. Your body weight matters too. Being overweight or obese can cause your body to produce more LDL and reduce your HDL, making it harder to keep your arteries clear.
Some people are born with gene variants that make their bodies naturally produce or keep more cholesterol than normal. This means they may struggle with high cholesterol no matter how healthy their lifestyle is. That’s why understanding your DNA and your genetic makeup can be such a powerful tool. It can help explain how your body handles cholesterol and guide you toward the most effective way to manage it.
How Your DNA Affects Cholesterol
Your DNA has a major influence on how your body handles cholesterol. While lifestyle choices like diet and exercise are important, some people are born with genetic makeup that makes it harder to keep their cholesterol levels in a healthy range. One example is hypercholesterolemia (FH) which occurs often from a young age, and increases the risk of early heart disease. But FH is just one example. There are many other ways your genes can affect cholesterol. Here are a few of the most important ones:
- Cholesterol absorption in the intestine: Some people have gene versions that cause their bodies to absorb more cholesterol from food than others. Even if they eat the same meal as someone else, their blood cholesterol may rise more quickly.
- Liver function and LDL clearance: The liver helps clear LDL cholesterol from your blood. Certain genetic variations can reduce how well the liver performs this task, leading to higher LDL levels.
- Triglyceride levels: Triglycerides are another type of fat in your blood. Genes may influence how your body stores and uses these fats, which also affects your overall heart health.
- Statin response and side effects: Statins are common medications used to lower cholesterol. However, not everyone responds to them the same way. Some people may see great results, while others might experience side effects due to their genetic variation.
Understanding how these genetic factors affect your body can make a big difference in how you can manage your cholesterol.
Using Genetic Data to Manage Your Cholesterol Levels
Genetic information is only the first step. Once a genetic risk like familial hypercholesterolemia is identified, care can be personalized to manage your cholesterol levels:
- Healthier Eating: A diet low in saturated fats and high in fiber supports cholesterol control. Genetic insights can reveal who may benefit more from specific dietary adjustments, since some people remain at risk despite healthy eating.
- Regular Exercise: Physical activity raises HDL and lowers LDL. With genetic testing, doctors can identify patients who need stricter exercise goals to offset inherited risks.
- Quitting Smoking: Smoking damages blood vessels, worsening cholesterol-related heart risks. Genetic information highlights who is especially vulnerable to early heart disease, making smoking cessation even more critical.
- Family-Based Care: Because cholesterol-related genes are inherited, family members can also be tested. This screening ensures treatment and prevention reach everyone at risk.
- Education and Support: Lifestyle changes and medications work best when patients understand their genetic risks. Genetic information gives patients a clearer picture of why care is necessary, boosting motivation and long-term commitment.