
Disclaimer: This article is for informational purposes only and is not intended to diagnose any conditions. LifeDNA does not provide diagnostic services for any conditions mentioned in this or any other article.
Nitric oxide is a gas produced by the body, made from equal parts oxygen and nitrogen. Its primary job is to relax the blood vessels, allowing more blood, oxygen, and nutrients to flow to vital organs. This helps keep your heart and blood vessels healthy.
NOS3, or nitric oxide synthase 3, is an important enzyme in the body that helps produce nitric oxide. It is especially active in the blood vessels and the heart. NOS3 can be thought of as a “factory” inside the body, making nitric oxide to ensure smooth blood flow and proper heart function. The role of nitric oxide is protecting the endothelium, the thin layer of cells that line the inside of blood vessels. If the body doesn’t make enough nitric oxide, the endothelium may become damaged which may increase the risk of cardiovascular disease.
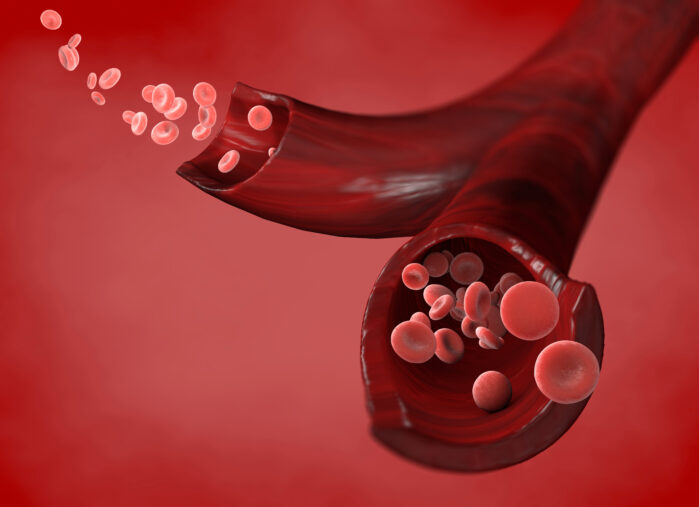
Nitric oxide or NO has several key jobs in the body, especially in the cardiovascular system (the heart and blood vessels). One of the main things NO does is to help relax the muscles in your blood vessel walls. When the blood vessel walls relax, they open up, allowing blood to flow more easily and reducing blood pressure. This helps maintain healthy circulation and prevents the heart from having to work too hard.
NO also has a protective effect by preventing the formation of clots inside the blood vessels. It stops platelets, the small cells that form clots, from sticking together, which lowers the risk of dangerous blockages. Additionally, NO keeps immune cells from sticking to the blood vessel walls, which is important for preventing inflammation and damage.
If the NOS3 enzyme doesn’t work properly, your body might not produce enough nitric oxide. This may lead to several problems, such as high blood pressure (because your blood vessels don’t relax as they should) and an increased risk of heart disease. There are also specific changes in the NOS3 gene that may affect how well it works, and these changes are linked to a higher risk of heart problems.
There are several genetic variations (known as SNPs or single nucleotide polymorphisms) in the NOS3 gene that can impact its function:
A study explored how genetic variations in the NOS3 gene, which plays a role in blood vessel function by producing nitric oxide, may influence the risk of heart problems and the effectiveness of certain medications. One particular variation in the NOS3 gene, -690 C>T (rs3918226), was associated with a slightly increased risk of coronary heart disease (CHD), a condition where the blood vessels supplying the heart become clogged. On the other hand , the -922 A>G (rs1800779), was linked to a slightly higher risk of heart failure, a condition in which the heart struggles to pump blood effectively.
The study also tested how three different blood pressure medications—amlodipine, lisinopril, and chlorthalidone—worked in people with these genetic variations. They found that for individuals with the -690 C>T variation, amlodipine was more effective than lisinopril at reducing the risk of stroke. For those with the Glu298Asp G>T(rs1799983) variation, taking amlodipine was linked to a lower risk of dying from any cause compared to those who took lisinopril.
The study suggests that genetic information may help doctors make better medication choices for patients, potentially reducing the risk of serious heart problems and improving health outcomes.
Recent research has explored how smoking might influence the connection between variations in the NOS3 gene and the risk of developing coronary heart disease (CHD) and ischemic stroke. The NOS3 gene plays a crucial role in producing an enzyme that helps keep blood vessels healthy. When there are genetic variations in this gene, it may affect blood vessel function, potentially increasing the risk of cardiovascular diseases.
The study involved 1,085 individuals with incident CHD, 300 with ischemic stroke, and 1,065 healthy participants. The researchers focused on two additional specific genetic variations in NOS3: the T-786C (rs2070744) and E298D (rs1799983) polymorphisms. They examined how these variations interacted with smoking history to affect the risk of heart disease and stroke.
The study found that the risk of CHD was higher in smokers carrying the E298D variant of the NOS3 gene. Specifically, smokers with the D298 allele were more than twice as likely to develop CHD compared to nonsmokers who carried two “normal” E298 alleles. This highlights the heightened risk of cardiovascular disease for smokers with this specific genetic variant.
In African-Americans, the T-786C genetic variation was associated with an increased risk of ischemic stroke, especially in individuals who had a long history of smoking (20 or more pack-years). Smokers carrying the C-786 allele were at a significantly higher risk of stroke than those with fewer smoking years or nonsmokers.
This suggests that both smoking and certain genetic variations in the NOS3 gene may add up together to increase the risk of developing heart disease and stroke. The findings highlight the importance of considering both genetic factors and environmental factors like smoking when assessing cardiovascular health risk. Understanding how these factors interact could help in identifying individuals at higher risk and tailoring preventive measures more effectively.


