
Disclaimer: This article is for informational purposes only and is not intended to diagnose any conditions. LifeDNA does not provide diagnostic services for any conditions mentioned in this or any other article.
As we age, certain changes inside the heart can quietly affect how well it pumps blood. These changes often go unnoticed until they begin causing symptoms or are discovered during routine checkups. In some cases, they result from health issues that develop in middle age or from rare conditions present at birth.
One common issue that can arise from these hidden changes is the narrowing of one of the heart’s main valves. This narrowing puts extra strain on the heart, making it harder to pump blood to the rest of the body. Over time, this may lead to symptoms like shortness of breath, fatigue, chest pain, or more serious complications. Understanding what causes Aortic Stenosis and how it progresses is key to managing it effectively.
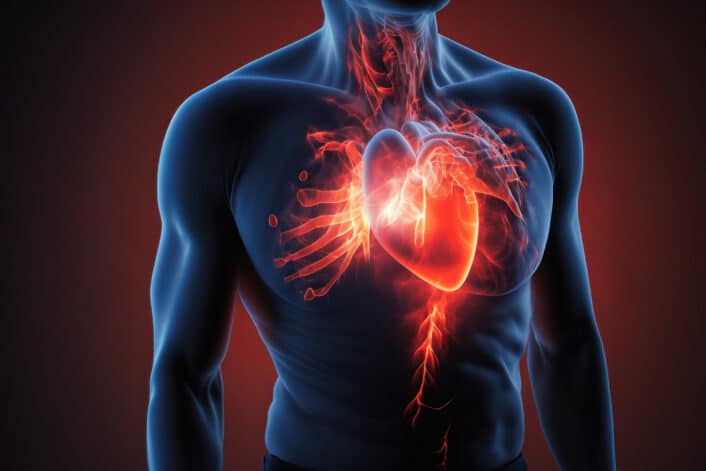
Aortic stenosis (AS) is when the aortic valve, one of the main valves in your heart, becomes narrowed or stiff. Normally, this valve opens and closes with every heartbeat, letting blood flow from the left side of the heart (left ventricle) into the aorta, which carries blood to the rest of the body.
In AS, the valve doesn’t open fully. This makes it harder for the heart to pump blood through it. Over time, the heart has to work harder to push blood out, which can lead to heart muscle thickening, fatigue, shortness of breath, and eventually heart failure if not treated. AS can happen for different reasons, including birth defects or age-related wear and tear. That’s why physicians say it can be either congenital (from birth) or acquired (developed later in life).
Congenital Aortic Stenosis: This type is something people are born with. The most common cause is called a bicuspid aortic valve, where the valve has only two flaps (cusps) instead of three. Because of this unusual shape, the valve can become stiff and narrow earlier in life. There is an even rarer condition having a valve with only one flap, and this usually causes even more serious problems and symptoms at a younger age.
Acquired Aortic Stenosis: This type usually happens as people get older. It occurs when a normal valve with three flaps slowly becomes stiff and narrow because of calcium building up on it. This process is often caused by aging and lifestyle factors like high blood pressure, high cholesterol, and smoking.
Aortic stenosis (AS) may often go unnoticed for many years because early on, the narrowing valve may not cause any obvious problems. However, as the valve becomes more restricted, symptoms typically start to appear, especially during physical activity. Common signs to watch for include:
These symptoms often signal that aortic stenosis has progressed to a moderate or severe stage. If left untreated, severe AS can become life-threatening, especially once symptoms appear. Early recognition and medical evaluation are crucial to managing the condition effectively.
Aortic stenosis happens when the valve that controls blood flow from your heart to the rest of your body becomes narrow or stiff. This narrowing makes it harder for your heart to pump blood, which may lead to symptoms and heart problems.
There are several reasons why this valve may become damaged or narrowed over time. Understanding these causes helps explain how aortic stenosis develops and why it affects some people more than others:
The congenital bicuspid aortic valve (BAV), a common congenital heart valve condition where the valve has two flaps instead of three, is highly genetic, with heritability estimated as high as 89%. However, this condition is not caused by just one gene but likely involves multiple genes and environmental factors.
Research has identified mutations in several important genes linked to BAV, such as NOTCH1, which is involved in valve development and calcification, and the GATA family of genes (GATA4, GATA5, GATA6), which also influence valve formation. Mouse studies show that altering these genes affects valve development and can cause BAV or related heart problems.
BAV changes the blood flow through the valve, creating abnormal stress that causes early calcium buildup and valve stiffening, which can lead to aortic stenosis (AS) and enlargement of the aorta. This calcification is an active process, similar to bone formation, involving cells in the valve turning into bone-like cells. The abnormal blood flow in BAV patients causes increased wall stress in the aorta, which differs based on the specific BAV subtype, leading to variations in how quickly calcification and valve disease develop.
Apart from BAV, acquired AS occurs later in life, mostly due to age-related calcium buildup on a normal valve and other cardiovascular risk factors like smoking, high cholesterol, and high blood pressure. This degenerative calcification is complex and likely requires multiple risk factors to cause significant valve damage.
Simply lowering cholesterol may not be enough to stop or reverse valve damage once it has progressed, highlighting the need for more personalized and combination therapies.
Diagnosing aortic stenosis usually starts when a doctor hears a heart murmur during a routine check-up. A murmur is an unusual sound made by blood flowing through a narrowed valve.
To confirm the diagnosis and understand how severe the stenosis is, doctors use several tests, including:
Early diagnosis is important because it helps doctors monitor the condition and decide when treatment may be needed to prevent serious complications.
Treatment depends on how serious the narrowing is and whether you have symptoms.


